The NBDHMT is a non-profit certifying organization designed to meet the clinical, technical and safety needs of the discipline of undersea and hyperbaric medicine. Opportunities exist for certification as a Diver Medic (DMT), as a Hyperbaric Technologist (CHT), and as a Hyperbaric Nurse (CHRN).
Whether you are preparing to take one of these certification examinations, or find it time to re-new, you will find a great deal of helpful information and guidance within the pages of our site.
The Board welcomes any questions or comments you may have. Use the “Contact Us” link to let us hear from you. Be sure to read the “Monthly Briefing” page, where regular updates on Board activities and related news are featured.
Mission
Ensure that the practice of diving medicine and hyperbaric oxygen therapy is supported by appropriately qualified technologists and nurses, through respective board certification pathways.
Purpose
Define and promote the safe application of diving medicine and hyperbaric oxygen therapy.
- Establish standards for introductory training course curriculum
- Develop, administer and evaluate technologist and nurse certification programs
- Promote professional development
Position Statements
Physician attendance and supervision of Certified Hyperbaric Technologists (2025-1) October 2025 (Rev. November 2025)
It is the position of the National Board of Diving & Hyperbaric Medical Technology that a hyperbaric medicine trained provider (MD/DO/NP/PA) must be immediately available to personally attend and support the certified hyperbaric technologist (CHT) during hyperbaric chamber operations. For hospital-based facilities, availability should be consistent with the CMS Federal Register final rule (November 20, 2009), Medicare Administrative Contractor (MAC) expectations, and others who purchase health care, for hyperbaric physician supervision, whereby the provider does not have to remain in the hyperbaric facility throughout the treatment but must be able to arrive within five (5) minutes of being summoned. In this situation, the hyperbaric provider should not be involved with patient care elsewhere that may cause them harm if immediately abandoned. For non-hospital based/private hyperbaric medicine practice, the provider must remain physically present within the office/clinical facility throughout the time the CHT is operating the chamber.
Safe Management of Monoplace Chamber Patient Thermal Comfort (2024-2) April 2024
It is the position of the National Board of Diving & Hyperbaric Medical Technology that monoplace patient thermal comfort is most safely managed by manipulation of the chamber’s gas (oxygen) flow/purge rate. This contrasts with providing an additional blanket(s) for patients who complain of being cold. Increased amounts of combustible material were considered the difference between a fully contained monoplace chamber fire and an uncontained fire that resulted in multiple deaths and injuries. Lower flow rates reduce the “wind tunnel-like” cooling effect. Equally important, lower rates increase chamber relative humidity (RH). Oxygen entering the chamber is dry. When combined with high flow rates, that serve to eliminate patient insensible moisture loss, chamber RH is low and has been recorded at 28%. This relatively dry environment is conducive to static electricity accumulation, the discharge of which is a fire risk in the presence of volatile hazardous vapors. Lower chamber flow rates allow accumulation of insensible moisture loss resulting higher RH levels (recorded in the 60’s) which act as a natural conductor to earth of any developing static charge. Further, objects do not hold a static charge quite as well at higher RH levels. For patients who complain of being too warm, a sheet rather than a blanket should be provided, and chamber flow proportionally increased. Room temperature can also be adjusted within the commonly recommended 68-72 F range to further promote thermal comfort.
Persons Qualified to Oversee Multiplace Chamber Fire Suppression Systems (2024-01) March 2024
It is the position of the National Board of Diving & Hyperbaric Medical Technology that multiplace hyperbaric chamber fire suppression system inspection, maintenance and testing is most effectively conducted by individuals who have undergone formal training in hyperbaric medicine and related safety, have completed hyperbaric safety director training, have achieved hyperbaric certification, and are authorized to undertake this responsibility by hyperbaric program leadership. Such individuals are considered by the Board to meet the definition of a “Qualified Person”, as referenced within National Fire Protection Association 99 Chapter 14 2024 14.3.4.3.5.5. The Board’s position is consistent with the NFPA definition of a Qualified Person, namely one who possesses a recognized degree, certificate, professional standing, or skill and who, by knowledge, training, and experience, has demonstrated the ability to deal with problems related to the subject matter, the work, or the project.
Certification in Hyperbaric Technology and Hyperbaric Nursing (2022-01) June 2022
Diver Medic Invasive Skills Requirement (2018-01) April 2018
It is the position of the National Board of Diving & Hyperbaric Medical Technology that the diver medic must receive training and skills necessary to undertake medical control physician ordered invasive procedures. Required skills are identified in Appendix II of the Certified Diver Medic “Approved Training Course Outline”. The Board expects that once acquired, such skills will be maintained through periodic updating, consistent with both the National Board of Diving & Hyperbaric Medical Technology recertification requirements and those of the medic’s employer/medical control physician.
Last reviewed 09/2022
Fitness to Work in Pressurized Settings: (2012-01) July 2012
It is the position of the National Board of Diving & Hyperbaric Medical Technology that every individual employed as a multiplace chamber inside tender, and all those who might otherwise be required to enter the pressurized chamber, be medically cleared as fit to work in this unique environment. The precise scope and extent of such screening examinations will be consistent with both prevailing standards and any recommendations from authoritative bodies. Interval repeat screening assessments should be conducted consistent with prevailing standards and following injury or illness that might influence subsequent medical fitness. Records documenting screening assessments should be maintained within each facility’s Human Resources/Personnel files as appropriate, and for a period of time consistent with prevailing regulations.
Failure to undertake such medical fitness screening is considered by the National Board of Diving & Hyperbaric Medical Technology to represent a fundamental breach of hyperbaric operational safety.
Last reviewed 09/2022
Safety During Multiple Occupancy Monoplace Chamber Operations: (2011-02) July 2011
It is the position of the National Board of Diving & Hyperbaric Medical Technology that whenever two persons occupy a Class B ‘monoplace’ hyperbaric chamber, individual grounding and air breathing capabilities should be provided to both occupants.
Class B chambers are designed for single occupancy in accordance with the National Fire Protection Association – NFPA 99. From time to time, however, a hyperbaric physician may require that a particular patient be accompanied during their monoplace chamber-based treatment(s). A common example is the pediatric patient who is not being mechanically ventilated. These patients may be accompanied by either a staff member or a family member, depending upon several variables. Hyperbaric textbooks and other publications feature numerous photographic examples of this practice pattern.
It is not the intent of the National Board of Diving & Hyperbaric Medical Technology to condone this practice, or otherwise. Rather, the Board recognizes that this practice does occur and wishes to ensure that appropriate safety measures are employed.
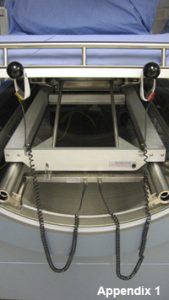
Both occupants should be directly grounded, the manner of which should be in accordance with NFPA 99 Chapter 14. An example photographic illustration is attached as Appendix 1. Consistent with the Board’s position on intermittent air breathing (Position Statement 2009-04, August 2009), both occupants should be provided with an individualized air breathing capability. An example photographic illustration is attached as Appendix 2.
Last reviewed 09/2022
Portable, Fabric, Low-pressure Hyperbaric Chambers: (2011-01) April 2011 (Rev. November 2016)
It is the position of the National Board of Diving & Hyperbaric Medical Technology that the design, fabrication and common use of portable, fabric, low-pressure (operating at pressures of no greater than 1.4 ATA) hyperbaric chambers is inconsistent with recognized and prevailing safety codes and standards.
The operational design pressure of a hyperbaric chamber that encloses a human within its pressure boundary falls within the scope of the American Society of Mechanical Engineers Pressure Vessels Human Occupancy 1 (ASME PVHO 1-2012). Portable, fabric, low-pressure chambers do not comply with this important safety code.
These chamber types are cleared by the Federal Drug Administration (FDA) only for the treatment of acute altitude (mountain) sickness and only when compressed with air. However, they are widely promoted for a large number of ‘off-label’ conditions and are at further variance with the FDA’s clearance in that some are used with oxygen concentrators and other sources of oxygen (‘enriched air’). It is also apparent that these chambers are not always operated in a manner consistent with the standards of the National Fire Protection Association (NFPA) 99 chapter on hyperbaric facilities.
It is the position of the National Board of Diving & Hyperbaric Medical Technology that portable, fabric, low-pressure hyperbaric chambers be limited in their use to the treatment of acute altitude sickness and that they be compressed only with air. Further, these chamber types should be designed, fabricated and operated in a manner consistent with prevailing codes and standards.
Last reviewed 09/2022
On-Line Introductory Training in Hyperbaric Medicine: (2010-02) October 2010 (Rev. September 2022)
It has been the long-held position of the National Board of Diving & Hyperbaric Medical Technology that introductory training in hyperbaric medicine must be undertaken in face-to-face classroom or seminar type settings. The NBDHMT recognizes the value of on-line education as a means of maintaining and advancing knowledge and skills. Such recognition does not extend to the learning of an entirely new field of medicine, technology, and related safety.
Given the current pandemic, the Board now allows introductory training to be delivered virtually. All currently approved courses intending to offer the virtual training option are required to undergo a real time audit to confirm that the delivery process and ongoing confirmation of student attendance meets the Board’s expectations. It is currently the intent of the NBDHMT to allow live virtual introductory training courses to continue indefinitely.
Physician Attendance and Supervision of Hyperbaric Oxygen Therapy: (2010-01) April 2010 (Rev. July 2013)
It is the position of the National Board of Diving & Hyperbaric Medical Technology that provision of hyperbaric oxygen therapy must be directly supervised by a physician (which includes a nurse practitioner/physician assistant where permitted by prevailing credentialing and regulatory standards) who is formally (UHMS or other authoritative body) trained in hyperbaric medicine, involving a face to face classroom vs. online setting. Such supervision should extend to:
- Assessment of suitability for HBO therapy
- Determination of risk-benefit profile
- Interpretation of any related diagnostic testing
- Generation of a therapeutic dosing profile
- Evaluation of subsequent clinical course, and
- Management of any related side effects and complications
Further, the hyperbaric physician must be on the premises and immediately available to the chamber facility at all times that the chamber(s) is occupied. Immediately available would meet the intent of this Position Statement if the physician could arrive at the chamber facility within five minutes of being summoned and in doing so, would not place in jeopardy any other patient presently under their care.
It is the duty of hyperbaric nursing and technical personnel to safely implement ordered therapy and closely monitor patients during their treatments. Should a patient voice complaints or manifest signs suggesting an unanticipated change in status, considered to be hyperbaric related or otherwise, the hyperbaric physician should be immediately notified. Importantly, hyperbaric nursing and technical personnel do not assume any of the physician responsibilities noted above and cannot initiate hyperbaric treatment without patient-specific hyperbaric physician signed medical orders.
Last reviewed 09/2022
In-home Delivery of Hyperbaric Oxygen Therapy: (2009-05) October 2009
It is the position of the National Board of Diving & Hyperbaric Medical Technology that the installation and provision of in-home hyperbaric oxygen therapy is inherently unsafe and cannot be condoned. The basis for the position is concern for the well-being of all such patients involved and the safety of those in proximity to the hyperbaric oxygen therapy delivery system.
In-home provision of hyperbaric oxygen therapy is likely to result in a bypassing of otherwise mandatory federal, state, and local codes as they relate to design, construction, installation, and operations.
In-home provision of hyperbaric oxygen therapy is likely to occur without adequate physician oversight and the operational support of appropriately trained and certified hyperbaric technologists and nurses. These shortcomings serve to further erode important safety standards.
Last reviewed 09/2022
Intermittent Air Breathing: (2009-04) August 2009
It is the position of the National Board of Diving & Hyperbaric Medical Technology that every recompression treatment facility and every clinical hyperbaric chamber, regardless of type or class, be equipped to provide intermittent air breathing. Intermittent air breathing, commonly referred to as an ‘air break’, serves to prophylax against and lower the incidence of, central nervous system oxygen toxicity. Intermittent air breathing also serves to treat pre-monitory signs and symptoms of oxygen toxicity, thereby reducing the potential for symptom progression to overt seizure.
The application and sequencing of intermittent air breathing will be at the discretion of the hyperbaric physician. However, intermittent air breathing should be immediately instituted (by either the multiplace chamber tender or monoplace chamber operator) whenever an acute change in patient status occurs and is consistent with, or suggestive of, CNS oxygen toxicity.
Last reviewed 09/2022
Hyperbaric Safety Director: (2009-03) July 2009
It is the position of the National Board of Diving & Hyperbaric Medical Technology that every recompression treatment facility and every clinical hyperbaric medicine service appoint a Hyperbaric Safety Director. This position is consistent with a previous NBDHMT Position Statement regarding adherence to recognized codes and standards. It serves to emphasize what the NBDHMT considers to be a key safety aspect. The Hyperbaric Safety Director should undergo formal and comprehensive training in the safety aspects of hyperbaric medicine and related technology. They should develop, maintain and manage a safety program based upon compliance with recognized standards. The resulting program should demonstrate effective elements of hazard mitigation, while employing recognized risk management concepts.
It is recognized that some hospitals and management companies with more than one hyperbaric facility appoint corporate safety directors. In these situations, an on-site safety director should also be designated. The intent is to have this individual be a full time member of each hyperbaric facility’s staff.
The term Hyperbaric Safety Director can be replaced with other titles of similar meaning and identical intent. Examples include Hyperbaric Safety Supervisor, Hyperbaric Safety Technologist, Lead Hyperbaric Safety Technologist, Hyperbaric Safety Manager, and Duty Hyperbaric Safety Technologist, and like terms. It is not the intent of the NBDHMT to assign a title. Rather, the intent of this Position Statement is to identify and emphasize the need for a trained and designated hyperbaric safety individual at each facility.
Last reviewed 09/2022
Recognized Hyperbaric Safety Codes and Standards: (2009-02) March 2009
It is the position of the National Board of Diving & Hyperbaric Medical Technology that the codes and standards expressed in the American Society of Mechanical Engineers’ safety Standard for Pressure Vessels for Human Occupancy (ASME PVHO-1)* and the National Fire Protection Association 99, Health Care Facilities Code, Chapter 14, (Hyperbaric Facilities)** be rigorously adhered to.
Using only hyperbaric chambers that have been designed, fabricated, tested and stamped in accordance with ASME PVHO-1 gives the user a high level of confidence in the quality and safety of the equipment in use and is an effective risk management tool. The use of hyperbaric chambers that do not meet these codes is strongly discouraged.
The installation and operational requirements found in NFPA 99, Chapter 14 have proven themselves since they were first issued in 1968. Not only does this standard provide guidance with regard to proper installation of hyperbaric chambers, it clearly prescribes safe day-to-day safety procedures that all should adhere to.
One standard that is particularly important from a day-to-day perspective is the issue of acceptable clothing. NFPA 99 Chapter 14 mandates that only clothing, and linens, made of 100% cotton or a blend of cotton and polyester fabric is permitted inside the hyperbaric chamber. These items shall be provided by the treating facility or specifically approved for hyperbaric use by the safety director in accordance with NFPA 99, Chapter 14.
The NBDHMT adds that acceptable patient clothing worn inside the hyperbaric chamber must not contain pockets. The majority of hyperbaric fires over the past two decades have been the result of prohibited items (pocket warmers, cigarette lighters and cellular telephones, are examples) being taken into the chamber. Eliminating pockets will do much to eliminate the introduction of prohibited items.
Last reviewed 09/2022
* American Society of Mechanical Engineers Safety Standard for Pressure Vessels for Human Occupancy, 2002. www.asme.org
**National Fire Protection Association 99, Health Care Facilities; 2021. www.nfpacatalog.org
Hyperbaric Facility Accreditation: (2009-01) January 2009
It is the position of the National Board of Diving & Hyperbaric Medical Technology that every clinical hyperbaric medicine program (defined here as a facility not solely available for the treatment of decompression accidents) undergo a Hyperbaric Facility Accreditation Survey.
It is the position of the NBDHMT that hyperbaric facility accreditation represents an effective measure of operational quality, safety, and compliance. The survey process allows each hyperbaric medicine program to be recognized for its strengths and to employ strategies to overcome any identified weaknesses.
The NBDHMT believes that an accredited hyperbaric medicine facility offers its patients, staff, and parent organization the highest assurance of safety, compliance, and therapeutic effectiveness.
Last reviewed 06/2025
Copyright © 2025. National Board of Diving and Hyperbaric Medical Technology. All rights reserved.
NBDHMT · P O Box 758 · Pelion, South Carolina 29123, USA · 888.312.2770
The National Board of Diving & Hyperbaric Medical Technology is a not-for-profit organization recognized as tax-exempt under the United States of America Internal Revenue Code section 501(c)(3) to ensure that the practice of diving medicine and hyperbaric oxygen therapy is supported by appropriately qualified technologists and nurses, through respective certification pathways. Funding is generated solely through certification fees and sales of Board merchandise. The National Board of Diving & Hyperbaric Medical Technology does not host or receive funding from advertisers or any other forms of business.
The information provided on this site is designed to support, not replace, the relationship that exists between visitors to this site and health care professionals. Any information collected by this site, such as e-mail address, will never be passed on to any third party, unless required by law.
Google Analytics is a webmaster tool used to determine the devices used to access this website so the content can be properly coded to serve phones, tablets or desktops. It is also used to determine the number of visitors to assess load on the server. It is used soley for this purpose and not configured in any way to track or individually identify the visitors themselves and should not concern the visitor in any way.
Updated September 15, 2025
