Monthly Briefing Archive
Current Monthly Briefing
2024
Monthly Briefing June 2024
Many of you will be aware of an essential flooding of the market with hyperbaric chambers designed and built to no known/acceptable code or standard. Several models are manufactured here in the USA. Others are shipped from overseas and commonly escape Customs scrutiny by falsification of their true contents on Bill of Lading documentation. Examples include “stainless steel tank” and “inflatable bag”.
These chambers violate numerous rules, regulations and standards and are considered, among other things, a threat to the safety of occupants and those in proximity. At the present time oversight organizations such as the FDA have not been as active in their interdiction as many would like or expect. Given this situation it’s possible that some CHTs may be unwittingly, or otherwise, involved in the operation of these unapproved chambers. Among other things, this would represent a violation of their CHT Code of Conduct attestation. Recently, a CHT was found to have gone as far as to train lay personnel in their operation, resulting in revocation of his CHT status.
There is sufficient concern within the Board that we are planning to introduce mandatory continuing education addressing this issue. It will take the form of 1.5-2.0 hours of Category A credits that comprehensively review standards related to chamber design, manufacture, interconnection and operation. The Board is most grateful for the shared expertise of Jim Bell, Francois Burman, and Andrew Melnyczenko who have kindly agreed to generate the necessary material. A launch date of January 1, 2025, is anticipated. We are considering the frequency at which this requirement should be repeated during recertification cycles and will let you know our decision in a future Briefing.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing May 2024
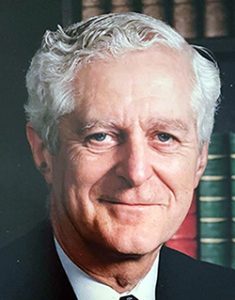
A little bit of hyperbaric history has recently been re-written. It has long been assumed that the first alteration in atmospheric pressure for therapeutic purposes occurred during the 17th century, under the direction of the English physician Nathanial Henshaw. He is said to have had constructed a chamber capable of hyper- and hypobaric pressures in which he treated several acute and chronic conditions, respectively. It was also said that those in good health might optimize their well-being by occasional visits to his chamber. This belief has been handed down over the ages without thoughtful analysis of its veracity.
In a recently published paper (May 2024) I conclude that his “Domicile” was nothing more than a proposal and argue the impracticality of such construction in that era. The paper is attached below. Those who speak on hyperbaric medicine’s history and agree with me will need to edit their presentations accordingly.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing April 2024
A monoplace-based hyperbaric safety director recently contacted the Board. She advised that her policy is to limit the amount of combustible material entering the chamber, including only allowing a single blanket. She added that her facility is currently treating a patient who insists on three blankets. Upon explaining why this is not permissible from a safety perspective the patient requested to speak to her medical director. She sought the Board’s guidance which was supportive of her policy and summarized below.
Limiting in-chamber combustible material should be an essential element of any fire safety plan. In the event of a monoplace chamber fire, it will continue to burn (while generating heat/increasing pressure) until either all combustible material is consumed, or the chamber’s internal pressure limit is exceeded, with resultant catastrophic failure. Excessive combustible material was considered contributory to the February 1996 uncontained monoplace fire and explosion in Yamanishi, Japan. There existed a relatively large “fuel” burden, in terms of the patient’s own clothing, including a heavily insulated acrylic jacket, along with blankets and linens. This contrasted with a fully contained monoplace chamber fire, also in Japan several years earlier, that did not involve the same amount of combustible material. The ignition source of these two fires was a reusable and a disposable pocket warmer, respectively.
Thermal comfort within a monoplace chamber is best addressed by manipulation of its oxygen flow/purge rate. If a patient complains of being cold, flow should be reduced thereby limiting the “wind tunnel-like” cooling effect associated with higher gas flows, rather than providing an additional blanket(s). This process has long proven effective and will be more so today with the lower available flow rate options. An additional advantage of a lowered flow rate is its impact on relative humidity (RH). The common source of compression gas is a bulk liquid system. Stored liquified oxygen passes through vaporizer coils and “boils off” to a moisture-free gaseous state prior to entering the chamber. This results in a low chamber RH (we measured it as low as 28% at 400 lpm). The dryer the atmosphere the greater the potential for static accumulation, a fire risk with any static discharge in proximity to volatile hazardous vapors. Reducing the flow rate to 240 lpm (the lowest available level in earlier chamber models) increased RH to the mid-60’s as patient evaporative moisture loss readily accumulates. Higher RH’s also act as a natural conductor to earth for any developing static charge while doing much to prevent its buildup in the first place.
Room temperature can also be adjusted upwards within the commonly recommended 68-72 F range if there are consistent complaints of patients being too cold.
For patients complaining of being too warm, provide a sheet not a blanket and increase flow rates to achieve the desired cooling effect, while accepting a proportionally lowered RH. Alternatively, adjusting room temperature to the lower and of the above range may prove sufficient.
The above summary has been condensed into the Board’s most recent Position Statement, at www.nbdhmt.org
Dick Clarke, President
National Board of Diving & Hyperbaric Medicine
Monthly Briefing March 2024
A hyperbaric technical/safety director notified the Board of a recent issue and requested we share it with the wider hyperbaric community. It relates to multiplace chamber fire suppression system oversight. His facility was visited by a representative of the city’s Fire Marshal, during which it was stated that inspection, maintenance and testing of hyperbaric chamber fire suppression systems can only be conducted by an independent qualified third party. This contrasts sharply with the long-established practice of members of the hyperbaric program being responsible for these tasks. As an authoritative source document, the representative cited the International Building Code, one which applies principally to construction of buildings, per se, rather than addressing items of equipment that may be installed within them. It is unlikely that a building sprinkler installer, as referenced within the code, would have requisite knowledge and expertise to capably address the unique aspects of multiplace chamber fire suppression systems. In a formal response to the Fire Marshal’s office, the facility’s management drafted a ‘Class “A” Multiplace Hyperbaric Fire Suppression System Compliance Report’. This document, which argues for fire suppression system oversight to remain ‘in-house’, awaits the Fire Marshal’s response. We will update you once a reply is received.
This issue prompted the Board to generate a Position Statement, one that advocates for fire suppression system operational oversight to remain the responsibility of qualified hyperbaric team members. The Position Statement is below.
“Persons Qualified to Oversee Multiplace Chamber Fire Suppression Systems (2024-01) March 2024
It is the position of the National Board of Diving & Hyperbaric Medical Technology that multiplace hyperbaric chamber fire suppression system inspection, maintenance and testing is most effectively conducted by individuals who have undergone formal training in hyperbaric medicine and related safety, have completed hyperbaric safety director training, have achieved hyperbaric certification, and are authorized to undertake this responsibility by hyperbaric program leadership. Such individuals are considered by the Board to meet the definition of a “Qualified Person”, as referenced within National Fire Protection Association 99 Chapter 14 2024 14.3.4.3.5.5. The Board’s position is consistent with the NFPA definition of a Qualified Person, namely one who possesses a recognized degree, certificate, professional standing, or skill and who, by knowledge, training, and experience, has demonstrated the ability to deal with problems related to the subject matter, the work, or the project.”
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing February 2024
This month’s Briefing was prompted by an email from a concerned CHT inside attendant. Included in her correspondence were elements of her medical record that served to corroborate much of what she wrote.
One well-appreciated risk of multiplace chamber staffing is decompression sickness. Its overall incidence is low, commonly reported to be less than 1%, with incidence defined as number of cases that occur divided by number of chamber exposures, or the potential for a case to occur during any given exposure. An inside attendant’s (IA) cumulative risk, defined as number of cases that occur divided by number of inside attendants, or the potential for an IA to suffer DCS, however, is not as low. Published reports indicate a range up to as high as 80%. Reference 1 below is an article that summarizes incidence, risk, and all-important mitigation strategies.
The CHT in question expressed concern about how her post-decompression complaints were addressed. She advised that she experienced “bends symptoms on several occasions.” Being new in her position she initially didn’t report them as she did not have health insurance. She reported subsequent complaints to the hyperbaric physician who advised her to see her primary care physician. Instead, the CHT notified an occupational health and safety nurse who referred her to the ED. Following a comprehensive workup she was diagnosed with “an impression of decompression sickness” and scheduled for an occupational health physician appointment three days later (accounting for the intervening weekend). While she was essentially asymptomatic during this next appointment, the assessment was again “Decompression sickness/illness. With skin symptoms plus neurological symptoms.” During a follow-up Occupational Health appointment, it was recommended she be considered permanently unfit for future IA employment, a decision she was willing to accept. At no time did there appear any discussion regarding missed therapeutic recompression opportunities. The CHT added that she did not undergo a fitness to work in pressurized settings assessment upon hire nor periodically thereafter.
There are several messages one can take from all of this, including what might represent related hyperbaric facility policies.
- Fitness to work in pressurized settings screening should occur at the time of hire and periodically (annually?) thereafter. It is also recommended screening occur after return to work/recovery from illness and injury. Screening procedures should be guided by the “UHMS Medical Fitness to Work Guidelines for Multiplace Inside Attendants”. Reference 2.
- There should be an established policy within the pre-treatment checklist that determines the current health status of the IA prior to their entering the chamber. An informed decision can then be made as to immediate pre-exposure fitness. Apparently, this did not occur in a published case involving an IA subsequently determined to have suffered a head cold and ongoing sinusitis. She experienced ascent barotrauma involving fracture of her right maxillary bone that remained undiagnosed for three days (while remaining at considerable risk for meningitis and some risk for brain abscess). Reference 3.
- Another policy provision should require formal determination for health status upon completion of every decompression and incumbent on IAs to report any change in status at this time, regardless of how minor it might seem and whether health insurance is in place. The IA should not be the one to diagnose their symptoms. In one very telling case, an IA exited the chamber, began to cough, and felt generally unwell. She was also quite tired from a long overnight treatment of a diver and wanted to go home to sleep. She was allowed to immediately leave without formal assessment and was found deceased at home an hour or so later. Autopsy was significant for overwhelming DCS. This case is discussed in Reference 1.
- Having IAs remain in proximity of the chamber for a given period post-decompression is another recommended policy. While somewhat arbitrary, at least 30-60 minutes would seem reasonable.
- A high index of suspicion should exist for any post-decompression complaints consistent with DCS. If symptomatic, the IA should be formally assessed by a hyperbaric physician at that time, rather than referring the IA elsewhere, where knowledge of decompression accidents may be scant.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing January 2024
The Board received an email earlier this week from an experienced CHT enquiring about any data that might be available regarding long-term effects on inside attendants (IA). She noted that she has worked in both multiplace and monoplace settings over a 20-year period and was unable to find any such information during an internet search. She added that beyond her personal interest, “many other CHTs along with patients have asked but I always come up with nothing”.
While this topic is not something that has garnered a great deal of formal research attention, there are an increasing number of recent publications, mostly in the form of retrospective analyses from single institutions. Another report represents more expansive survey and there are at least two related literature reviews. All of these are attached to this briefing, and I’ll briefly summarize them while referring to their article code (from my library).
Pulmonary function was studied by researchers in Turkey (673-019 & 673-001), Thailand (673-012) and Norway (673-002). Three of the four papers reported mean decreases of unknown clinical significance, the fourth found no short-term lung function deterioration.
One paper sought to determine the incidence of hyperintense brain lesions compared to controls with MRI imaging. (054-166) This small study of ten individuals in each group (none of whom had a history of any cerebrovascular, cardiovascular disease, or diabetes) revealed three lesions in two of ten IAs and none in controls, which was not a statistically significant difference. No disease was detected in the two IAs during detailed neurological exams. The authors helpfully summarized hyperintense brain lesion reports in industrial compressed air workers and recreational divers up to their 2006 publication date.
MRI screening for dysbaric osteonecrosis (DON) in 12 IAs was undertaken by researchers in Istanbul, Turkey, none of whom had a history of DCS. (052-048) No bone lesions consistent with DON were found.
A survey of IA occupational accidents and injuries in French hyperbaric facilities found that 27% of respondents reported at least one injurious event during the six-year survey period. Barotrauma and DCS dominated. (672-016) The second literature review summarized all reported acute and longer-term adverse events. (673-010)
A 2017 literature review (673-007) addressed all published IA decompression sickness (DCS) reports, including two nurse fatalities, from the beginnings of clinical hyperbaric medicine through 2017. It distinguished its very low incidence vs. considerable individual risk and concluded with a series of risk mitigation measures. Since then, at least three case reports identified Type II DCS in IAs. (673-008; 673-014; 673-015). While one might argue DCS is not a long-term effect, per se, it is likely to impact long-term wellbeing and future IA employment if unsuccessfully treated, so included here for completeness.
Best wishes for a safe, enjoyable, and productive 2024.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2023
Monthly Briefing December 2023
The 2024 edition of NFPA 99 Health Care Facilities Code has been released, and the NBDHMT encourages all hyperbaric facilities to have a copy readily available. The NFPA (nfpa.org) offers free access to view their codes, but a printed copy allows you to highlight sections and write notes of interest in the document. Also, having a printed copy lets you quickly see the other applicable codes in health care such as Chapter 5 Gas and Vacuum Systems and Annex A, which offers explanatory information.
There are numerous important updates to this edition, but two changes of note apply to those of you who hold the title of Safety Director:
- The title of safety director has been replaced with safety coordinator to better represent the role’s functions. All the requirements of this role/title remain unchanged. Additionally, within NFPA 99’s Annex A note A.14.3.1.3.2, it is explained that the title is not important, but having someone of skill and knowledge assigned the role and responsibilities of hyperbaric safety, as outlined in Chapter 14 – Hyperbaric Facilities, is.
- The term hyperbaric was added before safety. Instead of the document stating: “the safety coordinator must …,” it now says, “the hyperbaric safety coordinator must…”.
It is important to remember the Centers for Medicare and Medicaid Services (CMS.gov) adopted the 2012 edition of NFPA 99, which means hospital accrediting bodies such as The Joint Commission and DNV will inspect facilities according to the 2012 edition. Still, as hyperbaric professionals, you should be familiar with the latest code updates.
Many thanks to board member Richard C. Barry, PhD, for generating this month’s Briefing.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
References:
Centers for Medicare & Medicaid Services. (2023). Adoption of the 2012 edition of the National Fire Protection Association (NFPA) 101 – Life Safety Code (LCS) and 2012 edition of the NFPA 99 – Health Care Facilities Code (HCFC). Retrieved November 29, 2023, from https://www.cms.gov.
NFPA 99. (2023). NFPA 99 Health care facilities code (2024 ed.). National Fire Protection Association.
Monthly Briefing November 2023
The October 2023 Briefing summarized the frequency at which various categories of continuing education can be repeated during each recertification cycle and referenced related educational settings. This month’s Briefing describes what represents the majority of “Category A” topics, in terms of required core knowledge and competencies. The list is by no means exhaustive so get in touch with the Board to see if other educational opportunities you come across may also qualify.
FIRE SAFETY
ASME-PVHO 1 and NFPA 99 codes and standards review. Fire extinguishing options and periodic testing. Oxygen system cleanliness. Basis for prohibited items; review and update. Review of chamber fires and lessons learned. Fire safety drills.
OPERATIONS
Air decompression tables. Inside attendant (IA) periodic health/fitness screening. IA fitness screening after illness/injury. DCI presentations and management. IA decompression procedures. Acrylic viewport/window inspection standards techniques. Treatment table options. Medical, nursing and operator/technical staffing standards. Medical gas and compressed air systems. System maintenance and servicing. Electrical safety. Critically ill patient management review. Biomedical support equipment. Hyperbaric mechanical ventilator review. Periodic system inspections. History of staff accidents and injuries; lessons learned. Transcutaneous oximetry.
OXYGEN TOXICITY
Risk factors. Monoplace chamber air breathing options. Presentations and management of CNS oxygen toxicity. Presentations and management of pulmonary oxygen toxicity.
EMERGENCY PROCEDURES
Medically related emergency drills. Non-medically related emergency drills.
PATIENT CARE
Plan of care. Compliant documentation. Pre- and post-treatment assessments. Absolute and relative contraindications review and update. Universal precautions. Lung, ear, sinus, dental and GI barotrauma. Implantable medical devices. Claustrophobia-confinement anxiety. The pediatric patient. The diabetic patient.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing October 2023
The Board has been asked for guidance regarding the frequency at which various categories of continuing education can be repeated, particularly within a given CHT recertification period.
As the term implies, continuing education is focused on advancing knowledge and skills through additional formal learning activities. Continuing education can also include topics and programs designed to maintain core knowledge and competencies, but its principal concept is to build upon that knowledge and skill set. One example of the latter would be attendance at an introductory/primary hyperbaric training course where fundamentals of chamber fire safety are discussed. After such training a chamber fire occurs and upon release of an investigative report a formal presentation is generated. Its likely focus would be to address factors that contributed to the fire and how effectively the fire and involved personnel were managed. Its continuing educational aspect would be in the context of what unique lessons were gleaned from this event and likely supplemented with additional emphasis on fire prevention.
Below are several education category types and allowable frequency for recertification purposes. If there are any other forms of education being considered, please contact the Board for specific guidance.
Introductory/Primary Hyperbaric Training Course: While the Board is yet to see repeat training during a recertification application, it would be reasonable to grant credits if it was. One consideration for those who might contemplate attending another 40-hour course would be to select an alternative provider to the one initially attended. While standardized content for course approval exists, there are likely differing presentation styles and extent to how each topic is dealt with. One repeat course would be approved for a given recertification period, with the applicant encouraged to seek out advanced knowledge opportunities during future recertification cycles.
Professional Development Meetings and Conferences: No limitations on frequency per recertification period are in place for these annual/other periodic diving and hyperbaric medicine programs that have been awarded NBDHMT credits, as content tends to change with each subsequent offering.
Professional Development Courses: Examples include Hyperbaric Safety Director, Acrylic Inspection, Hyperbaric System Maintenance, and self-paced on-line programs approved by the Board. Attendance at these courses will be recognized for each recertification period. Again, if one wishes to repeat any of the first three listed for subsequent recertification then selecting an alternative provider should one exist may offer additional value. Self-paced learning modules must involve differing topics for each subsequent rectification period.
Institution-specific safety meetings/in-service training/safety drills: Hyperbaric program personnel are encouraged to apply for approval prior to applying for credits for these in-house initiatives. Documentation of topic(s), presenter(s), and attendance records are required. Get in touch with the Board if you would like guidance on how best to develop this category of credits. We can share examples from those who have done an excellent job. Any/all these ongoing initiatives count for each recertification cycle.
Review of published articles or textbook chapters: There is obvious value in staying up to date with emerging information yet feature as a formal continuing education offering. For continuing education and recertification purposes the reading material must first be approved by the Board and post-review questions generated. Typically, four multi-choice questions are preferred with three correct answers required for awarding credit. A particular topic can only be submitted once per recertification cycle. Contact the Board if you are interested in any such reviews. We can suggest articles, guide the approval process, and help with question generation if necessary. The Board typically limits three literature review credits per recertification cycle.
When considering continuing education opportunities, first determine if they are Board approved. If not, ask the provider(s) to consider an application. Should it be granted, the Board can then help in the promotion of these opportunities on behalf of the provider.
If there are any questions related to all this contact Board headquarters. We will be pleased to help.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing September 2023
A series of recent events warrant a reminder of the obligations CHTs face as they relate to their Code of Conduct attestation. The Code of Conduct establishes a clear outline of what represents required personal behaviors relating to ethics, integrity, and honesty. It also addresses professional traits with respect to compliance with prevailing codes, standards, authoritative guidelines, and laws.
Several examples of behavior appearing to conflict with the CHT Code of Conduct have been brought to the Board’s attention. They include CHTs seemingly involved beyond their scope of practice, such as operating a hyperbaric chamber independent of a physician’s order and prescribed dosing protocol (essentially practicing medicine without requisite licensure). Another is a CHT operating a chamber under an ordered protocol but with no designated medical provider available during treatment to intervene should an adverse event occur. This event involved the CHT in question calling the Board to seek guidance for the predicament he found himself in. One more is a CHT operating a hyperbaric chamber not designed, or manufactured, or interconnected in accordance with prevailing codes and standards. Teaching and “certifying” individuals to operate non-approved chambers also fails the Code of Conduct attestation. A CHT publicly and purposely misstating facts regarding prevailing codes and standards for apparent monetary gain has also been identified.
Failure to comply with the Code of Conduct risks initiation of disciplinary proceedings. Where behavioral and/or compliance shortcomings are established, the Board’s action may range from formal reprimand to revocation of CHT status.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing August 2023
In a follow-up to last month’s Briefing, there is encouraging news to share. The NFPA Technical Committee on Hyperbaric and Hypobaric Facilities rejected a proposed Tentative Interim Agreement (TIA) that sought to exempt soft-sided low-pressure chambers from prevailing codes and standards, argued the existence of a code gap, and proposed edits to NFPA-99 to accommodate this chamber type. The TIA involved two components, one technical and related to the last sentence, the other an emergent aspect given an incorrect understanding that a code gap existed. The committee vote was 17-0 against both components, with the proposer given a July 26 deadline if they wished to appeal. I checked with the NFPA on August 1 and was advised that no appeal had been received. This is hardly surprising as it would be seemingly impossible to conjure up any additional arguments profound enough to materially alter this unanimous decision.
The sum of all this is to make it abundantly clear that soft-sided low-pressure chambers are and remain subject to ASME and PVHO standards. As there is no code gap, no emergent nature to the proposal was deemed to exist.
*************************************************************************
I’m pleased to announce that Mr. Bryan Sully has been elected to the NBDHMT Board of Directors. Bryan is an experienced commercial diver, paramedic, diver medic and project coordinator. His bio can be viewed on the board’s website.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing July 2023
There has been increased discussion in the past couple of years regarding soft-sided/inflatable low pressure chambers, much of it directed at, and within, the NFPA Technical Committee on Hyperbaric and Hypobaric Facilities. This chamber type contrasts with the soft-sided higher pressure SOS Hyperlite chamber that is designed and manufactured in full compliance with ASME-PVHO standards.
There are some who argue, incorrectly, that NFPA 99 does not address low-pressure chambers so new language is required to bring them into compliance. It’s important to emphasize here that NFPA standards exist for all monoplace chambers. NFPA 99 does not distinguish chamber design, fabrication materials, intended operating pressure, or compression gas. NPFA states quite simply that they are all “Class B-Human, single occupancy”. In terms of design and manufacture, ASME to its credit did not cave to threats to promptly approve these chambers or face legal action. ASME advised soft-sided low pressure chamber advocates that a code case process exists to apply for manufacturing approval. As noted above, ASME has already approved such a code case.
There is another disturbing feature regarding low-pressure chambers worthy of note. Many who market and operate them incorporate an oxygen concentrator, in violation of the FDA. Approximately 95% oxygen is, therefore, introduced to a chamber occupant’s face mask or nasal cannula. Proponents argue their data indicates the chamber’s atmosphere never exceeded 23.5% during testing. Simple gas flow physics dictates, however, that somewhere near the oxygen delivery device values must be considerably higher, so by definition, therefore, an oxygen rich atmosphere. It’s all a matter of where one chooses to place the sample line’s internal take-off point.
Two recent (2023) pressure vessel structural failures, causing serious injuries in Utah and five fatalities in the North Atlantic, should serve as an object lesson for why manufacturing codes and standards exist. In many cases these codes and standards are rooted in disasters past, so responsible individuals and organizations should be arguing for not against them.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing June 2023
Long-standing board member Kevan Corson recently submitted his resignation. Kevan is a well-known and likeable figure within the related disciplines of diving medicine and hyperbaric oxygen therapy. He entered the field back in 1974, as an EMT. During his army career in the decade that followed he qualified as a saturation diver and underwent special operations advanced medical training, among several other achievements. Upon entering the civilian space, Kevan gained CHT status in 1991 and from that point on was a ubiquitous presence within many groups and organizations and served on many related committees.
The NBDHMT owes Kevan a great debt of gratitude for his selfless service in support of its mission. Thank you, Kevan!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing May 2023
Most if not all readers will be aware of the upsurge in sales and promotion of hyperbaric chambers directed at non-hospital affiliated clinics, wellness centers and private home use. While several such clinics appear somewhat aligned with accepted clinical standards and FDA adherence, the vast majority are not. This latter category commonly employs the inflatable low pressure chamber. They are not built in compliance with prevailing design, construction, and installation standards, yet their manufacture and promotion continue unchecked, at least in the USA. North of the border the Canadian government recently banned their importation, marketing, sales, and use, making it a crime to do otherwise.
An increasing number of individuals and clinics have acquired small steel chambers capable of higher pressures. They are commonly manufactured overseas and likewise fall short of prevailing design and manufacturing codes and standards. To get these non-complaint chambers into the USA requires shipping agents to falsify their true nature to circumvent otherwise mandatory Customs inspections. I am presently looking at one such Bill of Lading that lists the commodity as “Stainless Steel Tank”. It was shipped from Shanghai, China to a certain hyperbaric clinic in California and slipped though the inspection process as intended.
Similar small steel single and dual person chambers are also produced in the USA. One manufacturer promotes them directly for lay person in-home use, noting that these are essentially “Do it Yourself” chambers with “controls located from inside only” on one version. The lay person selects size, occupant capacity, and what pressure relief valve to use, with ten to choose from! “Included is everything you will need to start your treatment protocol right from your own home except commercial oxygen ‘K’ size tanks that can be rented from your local supply house”. Earlier this week (today is May 25) one of this company’s chambers suffered an uncontrolled loss of pressure following an acrylic window failure. One occupant suffered pulmonary barotrauma with resulting pneumothorax, another suffered a ruptured tympanic membrane. It could have been much worse.
I’ll leave it to the FDA and others to hopefully address compliance and clinical futility, given many wholly unsupported claims of therapeutic effectiveness. Most concerning to me, beyond taking advantage of the gullible and the vain, is the issue of safety. Safety of unsuspecting (little in the way of meaningful informed consent) chamber occupants. Safety of those in proximity to these chambers. Operator (occasionally the patient themselves) training is clearly suspect. Issues related to the handling of HP oxygen cylinders, oxygen concentrators, managing oxygen system cleanliness and ability to monitor the chamber’s atmosphere are clearly concerning. So, too, issues related to maintaining and servicing these chambers.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing April 2023
The Board continues to receive calls and other forms of communication from CHTs who express concern that they frequently find themselves operating chambers in the absence of a hyperbaric physician. One CHT advised that he was told by the hospital’s contracted manager that if the physician plans to arrive at the hospital within 30 minutes he can immediately start treatments, as this was “policy”. No information was forthcoming as to exactly whose policy it was. It is certainly not that of any compliance organization the Board is aware of, nor that of government and commercial health insurers. A CHT sought the Board’s advice just last week. He operates two monoplace chambers at a small rural hospital in central Florida frequently in the absence of an onsite physician. He was likewise advised by his management company representative that this was acceptable. He wondered about the veracity of this guidance and whether it would adversely impact his CHT Code of Conduct attestation. In two recent cases no licensed health care provider undertook a patient assessment prior to initiating HBO therapy.
We thought it useful to review related compliance standards and I am grateful to board member Valerie Short for her following expert summary.
Before tasks can be delegated to unlicensed personnel such as CHTs, the level of critical thinking and scope of practice required for the tasks must be considered. Patient assessments are one area that cannot be delegated to anyone other than a Registered Nurse, or a provider. When services are provided within a hospital-based outpatient department, nursing assessments are required as part of Medicare’s Conditions of Participation for all patients, in addition to provider treatment and visit notes. LPNs and unlicensed personnel may assist with gathering data such as vital signs and blood sugars as a part of the pre-treatment assessment. However, the supervisory provider or an RN must evaluate the data and perform the other assessment aspects. An unlicensed person has no scope of practice that would allow them to independently perform a patient assessment and make determinations regarding the safety of treating a patient, which must be provided prior to initiating HBO therapy.
Regarding the presence of a physician, Medicare requirements published in the federal register for physician supervision of hyperbaric treatments changed from “direct” to “general” effective January 1, 2020. CMS emphasized that ultimately this change was due to supervision compliance being too difficult to monitor under Part A hospital billing and so they believed compliance was better monitored in other areas, such as the electronic claim process. It did not, however, change the requirement for physicians to participate in oversight of every hyperbaric oxygen treatment.
The descriptor for CPT code 99183 reads, “attendance (my emphasis) and supervision…”. CMS finds the definition of 99183 to be similar to an evaluation and management code. To meet the attendance aspect of the definition and report this service, the physician must personally provide some aspect of care to the patient. Whenever a claim is submitted for HBO, the system will audit for the presence of the technical service (G0277), as well as the supervision of the service (99183).
Medicare contractors have an expectation that the supervising provider will be in the department when the chambers are in operation for the duration of each treatment in off-campus or free-standing centers. For hyperbaric services in a provider-based hospital department, the regulations state that the physician must be present during chamber descent and ascent. During the remainder of the treatment they must be able to physically respond within 5-minutes. Additionally, the supervising physician must not be engaged in another patient care service that they could not immediately walk away from. For example, they could not be in the operating room, or the only physician covering the emergency room where they couldn’t immediately walk away without potentially jeopardizing another patient’s safety. These rules are all published in the Federal Register, as well as within Medicare Provider Manuals.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing March 2023
Humble apologies for the delay in producing a March Briefing.
You may be interested in several topics during the upcoming UHMS Mid-West Chapter meeting, May 6. One of which will ask the question “Is transcutaneous oximetry still relevant in the current era?”. I have agreed to take this on and plan to evaluate all point-of-care/bedside screening options for lower extremity lesions/DFUs in the context of respective strengths and weaknesses. There are several traditional tests you will be familiar with and a couple of others likely new to you. At the conclusion of the presentation, I will answer my own question.
For more information and registration details please contact the Society at www.uhms.org.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing February 2023
The primary function of the NBDHMT is to approve training courses that serve as a pathway for diving and hyperbaric medicine certification. The approval process is multifactorial and begins with the Board’s development of curriculum guidance based upon minimum educational standards. It extends to a review of teaching materials submitted by those seeking approval, and here the Board is prepared to spend all necessary time to overcome any considered shortcomings. Examples might include poor quality audiovisuals, outdated information, insufficient focus on current era clinical practice, operational and safety standards, misstated data, topics inconsistent with the required curriculum, and densely packed slides that presenters would presumably narrate verbatim rather than using them as teaching prompts. Once all materials are in order, the Board schedules a live audit of each course’s first offering. This is quite unique and something we are proud of as the Board is unaware of any other credentialing organization that commits such resources to confirm courses are being taught in a professional and effective manner.
Successfully delivered courses are provisionally approved, pending any final edits, and subsequently approved typically for a period of three years. At the time of re-approval, the Board will review the current program outline and likely to audit selected topics prior to ensure ongoing compliance.
Almost without exception, course directors express gratitude for the available expertise and comprehensive manner in which the NBDHMT undertakes course oversight and accreditation.
Most importantly, this review and oversight commitment strengthens the Board’s mission “To ensure that the practice of diving medicine and hyperbaric oxygen therapy is supported by appropriately qualified technologists and nurses, through respective board certification pathways”.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing January 2023
A little more dialogue here relating to the importance of ongoing skills and knowledge maintenance and updating. It adds to commentary found within the June 2020 Monthly Briefing where the need to consolidate existing knowledge and be exposed to updated operations and safety recommendations/standards, insightful accident/incident reports was emphasized.
For more than a decade the Board has required continuing education to be primarily focused on the roles and responsibilities of the CHT. Historically, there was little guidance and distinction as to what represented appropriate continuing education content. Attendance at any number of hyperbaric related meetings and related events would qualify for re-certification despite no direct employment relevance. In the 2020 Briefing it was noted that core educational content should address hyperbaric operations, related technical aspects and chamber system safety to the extent of a minimum of nine of the required 12 Category A recertification credits.
Examples of what might also constitute Category A credits include any material related to decompression sickness (an inside attended risk factor), cerebral arterial gas embolism (another risk for inside attendants as well as hyperbaric patients), barotrauma involving its many potential anatomic sites, inside attendant initial and periodic fitness screening, return to inside attendant duties screening after illness or injury, periodic hyperbaric department meetings with documented topics and attendance verification. If there is other material that you feel might qualify for Category A get in touch with Board headquarters to have them make a determination.
Dick Clarke, President
National Board of Diving & Hyperbaric Medicine
2022
Monthly Briefing December 2022
Many of you are likely aware of increasing numbers of free-standing clinics, lifestyle/wellness centers and even private citizens offering access to hyperbaric chambers. In doing so, they market and promote their services for any number of “off-label” conditions, as they do to others who are perfectly healthy but have been convinced that hyperbaric exposures (purposely avoiding the term treatment here) will make them healthier. All of this is in violation of Federal Drug Administration regulations. While mainstream hyperbaric medicine practitioners may occasionally treat a patient off-label should a reasonably sound mechanistic basis exist and alternatives are in short supply or high risk, think pneumatosis cystoides intestinalis, they don’t market their service for such an indication and certainly don’t base their practice on off-label uses.
There is another disturbing side to all of this. It involves the use of hyperbaric chambers that have not been cleared by the FDA and don’t meet manufacturing (ASME-PVHO-1) and installation (NFPA-99) standards. In most instances these chambers have been produced overseas and imported with shipping container manifests creatively manipulated to conceal their true contents to avoid Customs scrutiny. I’m sitting here looking at one such manifest that identifies two steel single person chambers delivered to an address in California from China as “Stainless Steel Tanks”. The FDA was presented with this and numerous other examples earlier in the year.
I did want to bring all of this to the attention of Monthly Briefing readers, especially CHTs. As a function of becoming certified, each CHT agrees to abide by a Code of Conduct. Knowingly working within/operating chambers that violate these regulations and standards serves to jeopardize that Code attestation and threatens one’s ongoing certification status.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing November 2022
Effective November 1 the Board’s mailing address has been changed. Please make note of this and direct all future written correspondence to the NBDHMT at Post Office Box 758, Pelion, South Carolina, 29123, USA. The previous address will be checked from time to time for the foreseeable future.
Also, effective immediately, examination scheduling dates will now be confirmed within 45 days rather than the previous 21 days of application. Workload constraints, in one instance last month involving as many as 15 testing sites on a single day, dictate that we extend the administrative management period.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing October 2022
In 2020, and given the constraints imposed by COVID-19, the Board approved live video teaching of introductory hyperbaric training courses “for the duration of the pandemic”. The Board did not, however, approve applications for online enduring materials/self-paced learning. In terms of subsequent CHT/CHRN certification testing results, there has been no measurable change in pass/fail rates, suggesting this alternate teaching approach has validity. Recently, the Board voted to indefinitely continue its approval of hyperbaric course livestreaming. Should the Board revert to an in-person requirement it will provide course directors with 120 days notification.
One drawback of virtual training is the issue of hands-on training. This has been solved, in part, with video demonstrations. To further account for this shortcoming students are encouraged to undergo formal preceptorship immediately upon return to their individual institution. Should they be associated with a new program, the chamber manufacturer’s installation representative will be expected to provide chamber operation fundamentals. Engaging a knowledgeable consultant may also be of value.
One marked advantage to this virtual approach has been the ability of the Board to enhance its course oversight responsibilities. Previously, a single representative would be on site for each new course, with attendant cost and time commitments. Being able to remotely view live presentations has allowed a sharing of audit responsibilities and elimination of burdensome travel. It has also allowed the Board to identify and advise of any variances in approved content “drift” by occasional spot auditing of established courses. Course directors are notified, where appropriate, of any requisite upgrading to maintain compliance with approval status. It has further allowed the Board to advise course directors of necessary/recommended upgrading based upon evolving clinical, operational and safety data.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing September 2022
It’s saddening to learn of yet another diving medicine luminary “crossing the bar” as one is apt to say in the Royal Navy (courtesy of Alfred Lord Tennyson 1817-1904), and an appropriate term here for Dr. Peter B. Bennett, who passed away on August 9, aged 91. Dr. Bennett was employed by the Royal Navy for two decades and it was there that he pioneered ultra-deep diving techniques, culminating in a world record simulated dive to 1,500 fsw, in 1970. He emigrated first to Canada, where he formed and headed the Defense and Civil Institute for Environment Medicine, and then to the US, and Duke University Medical Center. His research interests included nitrogen narcosis, oxygen toxicity, diver ascent rates and decompression sickness. He was the first to describe, and name, the adverse effects of helium-oxygen (heliox) mixtures, namely high-pressure nervous syndrome (HPNS). He is also credited with the invention of trimix breathing, when he added small amounts of nitrogen to heliox to “offset” the disabling effects of HPNS. While at Duke he oversaw the “Atlantis” series of dives, setting another world record with a dive to 2,250 fsw, taking 45 days to complete.
Dr. Bennett founded the Divers Alert Network and served as its president for many years before becoming Executive Director of the Undersea and Hyperbaric Medical Society, until his retirement 2014. He was recently pre-deceased by his co-editor of the highly regarded textbook Physiology and Medical of Diving, Dr. David Elliott (see the February 2022 Monthly Briefing). Dr. Bennett published five other textbooks and had some 200 scientific articles to his credit.
Peter B. Bennett, PhD, DSc. 1931-2022
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing August 2022
So called mild (1.4 ATA or less) hyperbaric chambers continue to proliferate at a seemingly unprecedented rate. They do so on the strength of promoting wholly unproven and in many cases implausible benefits to the desperate, the gullible and the vain. Most commonly, these chambers are of a soft-walled inflatable design but there are hard-shelled low-pressure versions out there as well.
Inflatable hyperbaric chambers are approved by the FDA based on “substantially equivalent” to the air-filled Gamow (pronounced Gam-of) Bag, pictured below. And approval is limited to treatment of “Acute Mountain Sickness (AMS) and its associated mild symptoms”. Readily apparent upon the most cursory of internet searches is that this chamber type is proposed as treatment, and I use this term loosely as it is an undoubted exercise in futility, for anything but AMS. Multiple occupancy utilization is not uncommon, another FDA violation, and one company manufacturers a four-person capability. Mild hyperbaric chamber operators and users further violate FDA approval when incorporating an oxygen breathing system.

Following a recent and concerted educational effort, State and Local Fire Marshals have begun closing businesses promoting mild hyperbaric oxygen therapy due to non-compliance with NFPA 99 Chapter 14 standards. One affected commercial enterprise reacted by proposing that because their inflatable chambers offer therapeutic not medical services and represent a lower risk than traditional hyperbaric chambers, they should not be held accountable to current standards. Further, they proposed a new NFPA category be developed specific to this chamber type. I was one of two individuals who offered public statements against these proposals during a August 1 NFPA meeting. My comments are attached in the following Word file.
Public Comment Regarding NFPA 99
Encouragingly, the NFPA Hyperbaric Facilities Technical Committee voted unanimously to reject both proposals.
In the week prior to that meeting, the American Medical Association formally opposed the use of the mild hyperbaric therapy…see link.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing July 2022
During the June 2022 Board of Directors meeting, several changes were agreed to regarding the CHT testing process. Effectively immediately, there is no longer a limit on the number of times the certification examination can be attempted. Previously, a three-test limit was in force at which point individuals would no longer be able to certify in hyperbaric technology if their third try also resulted in failure. This change brings the Board more in line with other medical technology certification organizations. In addition, the previously mandated six-month waiting period between tests has been reduced to three months. Should the period between formal hyperbaric training and retesting eventually exceed three years, proof of maintenance a qualifying pathway is required.
One final change is provision of a check box within the application form to request special accommodation for those with testing disabilities, such as dyslexia and testing anxiety. Such needs will be addressed on a case-by-case basis and may include approval for beta blockers to be prescribed and extra time beyond the otherwise standard two-hour test limit. Special accommodations will only be considered at the time of examination registration, i.e., not those raised at the time of testing.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Monthly Briefing June 2022
The Board’s annual directors meeting took place on June 17 via Zoom video conferencing. One order of business was to consider several new Board members. After careful deliberation, the three following individuals were elected, each having achieved the required majority vote.
LCDR Gary D. Montgomery, PA. Gary serves as Director of the National Oceanic and Atmospheric Agency (NOAA) Diving Medicine Program. His responsibilities extend to medical oversight of all NOAA diving medical officers and diver medics.
Gregory J. Brown, MBA, BS, AAS, CHT-ADMIN. Greg recently relocated from Duke University Medical Center to Regional One Health in Memphis, Tennessee where he serves as Program Director of hyperbaric medicine and wound care.
Jeffrey B. Nance, DMT, CHT. Jeff is the long-standing senior care provider at the University of Hawaii Multiplace Hyperbaric Treatment Center in Honolulu and provides PRN support at Queen’s Medical Center’s monoplace hyperbaric facility, also in Honolulu.
We are delighted to welcome these new members and are confident they will bring a wealth of knowledge and expertise to the Board’s mission and deliberations.
On a final note, will all of you who certified or recertified during this month of June please go to www.nbdhmt.org and the Confirm Certification link to ensure that your name is recorded. We are in the process of switching over control of the website and want to be sure we didn’t miss any updating.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2022
A note to recognize membership changes within the Baromedical Nurses Association Certification Board and give a shout out to Deb Critz, who both rotates off the Board and retires into her professional sunset after three plus decades as a hyperbaric nurse. Deb was one of the early CHRNs and contributed much to the BNA in its formative years and beyond. The NBDHMT extends its gratitude and best wishes to Deb for a “career well done”!
Kathy Nelson replaced Angela Savage earlier this year and Kari Fowler will replace Deb effective July 1, at which time Dan Christopher will begin serving the BNACB as it chair.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2022
A reminder for those of you who have a need to call Board headquarters (+1.803.434.7802). If one of our administrators does not pick up the phone, please listen to the recorded message in its entirety. This will allow us to better serve your needs and accelerate turnaround times. You will be instructed to either email (nbdhmt@aol.com) or fax (+1.866.451.7231) any documentation you have, and you may also leave a voice message, which will be promptly addressed.
Another reminder regarding the application process for NBDHMT training course approval. There is no reciprocity with other organizations that approve introductory hyperbaric training. The Board independently assesses all such applications. It begins with a review of faculty member qualifications and all related course materials and other documentation. Once any shortcomings have been rectified an audit of the live course is scheduled. This process has served to enhance approved course quality and validate the Board’s position regarding reciprocity.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2022
A reminder that the Board’s website includes a Career Center section. This is a useful resource for those looking to fill a position as well as qualified individuals seeking employment. Some two thousand CHT’s, CHRN’s and DMT’s are currently certified through the NBDHMT so a large potential audience for your staffing needs.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2022
Professor David H Elliott, OBE
1932-2022
It’s always a little sad to learn of the passing of someone who enjoyed great influence and presence in a particular field, and this certainly applies to Dr. David Elliott who died last month at age 89.
He spent 16 years in the Royal Navy (after an earlier three-year stint of mandatory national service) as a research scientist specializing in diving medicine. He was seconded to the U.S. Naval Research Laboratory for several years as an underwater medicine specialist with some aspects of his work benefiting NASA’s space program. During this period, he became a world-wide authority on decompression sickness. He authored many important publications and is perhaps best known for “The Physiology and Medicine of Diving” which he co-edited with Dr. Peter Bennett. Introduced half a century ago this was and remains the principal academic textbook in its field and now in its fifth edition. After leaving the navy he joined Shell Oil Company as its Chief Medical Officer, and it was here he played an important role caring for injured commercial divers in the North Sea and elsewhere. He was a sought after and entertaining speaker at many a diving medicine meeting and conference and was quick to don his diving gear and get into the water between lectures. Knowingly or not, all those who dive today benefit from his pioneering contributions to diving practices and related safety.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2022
Registration for the first of our diver medic refresher sessions of the year (February 4) has reached a remarkable 100. While most are indeed medics, several physicians, fellows, residents, CHT’s and CHRN’s have also signed up. In all they represent 11 countries, another impressive milestone.
On the clinical research front there is some news. Earlier this month the first randomized controlled clinical trial addressing HBO treatment of mandibular osteoradionecrosis based on the Marx Protocol was published (reference below). While many of you will be familiar with this long-standing management approach, the fact that it has never been formally verified as effective might surprise some of you. The 2004 Annane et al. RCT (also referenced below) attempted do so, but study design and conduct were woefully at odds with Marx’s algorithmic approach to localized/early stage ORN. This new report combined two small trials as both had struggled with recruitment. While there was a trend towards improved outcomes after surgical removal of bone in patients who received HBO vs. those who didn’t, the difference was not significant. The authors point out, however, that the study was underpowered (low vs intended recruitment) so this negative result is not statistically significant. They encourage further research on the effect of HBO for ORN as well as relevant alternatives and emphasize that no recommendation can be made for peri-operative HBO after ORN surgery on the strength of this study…likewise, no recommendation can be made to abandon HBO.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Forner L, et al. Hyperbaric oxygen treatment of mandibular osteoradionecrosis: Combined data from the two randomized clinical trials DAHANCA-21 and NWHHT2009-1. Radiation & Oncology 2022;166:137-144
Annane D, et al. Hyperbaric oxygen therapy for radionecrosis of the jaw: A randomized, placebo-controlled double-blind trial from the ORN96 study group. Journal of Clinical Oncology 2004;22:1-8
2021
December 2021
Not a whole lot to report from Board headquarters as we close out the year in which the pandemic finally appeared on the wane only for another variant to blunt our hopes.
Several FBI agents transitioned their DMT status to Public Safety Diver Medic last month. This better represents their primary role as supporting diving operations without immediate access to recompression facilities. Many thanks to Board member Dr. Sean Hardy and to Greg Barefoot, PA, for expertly providing the necessary lecture content to facilitate this change.
A reminder that your program’s periodic team meetings may qualify for Category A credits. Several facilities take advantage of this when they undertake well-constructed and well-documented safety and operational review update sessions. If you would like to see some examples as essential templates let us know.
Best wishes to you all for a safe and enjoyable holiday season.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2021
Our third and final diver medic refresher training session for the current year was held on October 28, 2021. A record seventy three registrants logged in via Zoom for a review and update on several requested topics. A number of hyperbaric personnel joined in to take advantage of presentations with relevance to clinical operations and safety, and earning CEU’s in the process. Four sessions have been scheduled for the coming year, the first of which will take place on February 4, 2022. As before, there will be opportunities for CHT/CHRN’s to ‘learn and earn’.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2021
The third in a series of half-day diver medic refresher training sessions during this current year is scheduled for October 28. While primary directed at the DMT, the planned material holds considerable relevance for the CHT and the CHRN. Accordingly, the Board has awarded 3 Category A and 1 Category B credits, and the South Carolina Nursing Board has awarded 4 CEUs. The full program and topic time frames can be found in the link below, as can the registration form.
Management of pneumothorax occurring within the hyperbaric chamber will represent the most extensive review and updating of this critical issue on record.
Diver Medic Refresher Training: Session Three 2021
(Virtual, per Zoom; October 28, 2021)
Diver Medic Refresher Training Application
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2021
Happy anniversaries, and plural indeed!
Next month begins the fourth decade of the Certification in Hyperbaric Technology program. The first CHT certificate was issued on October 17, 1991. Since then, 4,643 allied health professionals have successfully challenged the certification exam. Of that impressive number 1,155 remain certified/operationally active today.
This year also marks the 25th (silver) anniversary of the hyperbaric nursing certification program. Several of the Baromedical Nursing Association’s leadership undertook an essential audit of the exam in late 1995, with the CHRN program formally launched the following year. At this time of writing, 1,374 nurses have been certified over the past quarter century and 505 remain clinically active within the practice of hyperbaric medicine.
As a reminder, the NBDHMT as a certifying organization had its genesis in the world of the commercial/professional diver. Accidents and injuries were somewhat commonplace, and particularly testing to manage in the geographic and medical remoteness of the offshore oil and gas industry. When they occurred within a pressurized chamber complex related clinical management was additionally challenging, as there was invariably no on-site source of knowledge and skill. Common oil industry practice was to not allow their rig medics to pressure-up to treat an injured diver as it would require many hours, even days, before they could be safely returned to surface pressure, with 100 or more rig workers lacking access to urgent medical care in the interim. One exception I do recall was the good Charlie Duff, a highly respected pharmacist mate and barge medic. During one rotation in the Gulf of Mexico in 1969 Charlie entered a saturation diving chamber to spend more than 50 hours supporting a critically ill diver who had been almost completely eviscerated…utterly heroic stuff.
The diver medic certification program was the solution to sourcing an on-site “tip of the spear” diving accident management capability, with the National Board developing its curriculum, instructor accreditation requirements and eventual standardized DMT certification exam.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2021
I thought it helpful to use my recent blog as this month’s Briefing given its important safety message.
Hyperbaric Chamber Fires: Lessons Lost

Hyperbaric chamber fires continue to occur with troubling frequency and have been uniformly fatal since all six occupants survived the Geisinger Medical Center, Pennsylvania, fire in April 1989. As devastating as these events are, there have been disturbing consequences on more than one occasion. One example is a failure of those who would be expected to ensure independent expert investigation to actually do so. Alternatively, if one was undertaken, for some reason its relevant findings did not enter the public domain. I don’t know about you, but I can’t think of a single reason compelling enough.
Institutions and governments have a moral and an ethical responsibility to formally investigate these tragic circumstances and not censure findings, no matter how embarrassing they may be to some. Failing in this responsibility leaves the health care delivery system, particularly its hyperbaric community, to worry and wonder, and potentially important lessons are lost.
When transparency prevails, events (plural here as invariably there are several) that contributed to the outbreak of fire, attempts made to extinguish it, and efforts directed at rescuing chamber occupants, can be systematically analyzed. It is this process that’s likely to serve, among other things, as a vital “lessons learned” opportunity. Examples may include a given facility’s fire safety plan being subsequently considered validated when measured against the report’s findings. Alternatively, it may identify some room for enhancement within that plan. Perhaps it could determine one or more shortcomings in what was otherwise considered to be an adequate plan, and gaps promptly reconciled. It might prompt a decision to run a fire safety drill to test aspects of an existing fire safety plan related to factors implicated in a fire’s investigative findings. Finally, it could identify chamber as built/as installed/as interconnected issues, not previously recognized, thereby leading to a degree of system “re-engineering”.
 Clearly, much is to be gained when leaders act responsibly. When they don‘t, critical risk-mitigation measures are likely to go unaddressed or unenforced and the well-being of tomorrow’s hyperbaric patients and staff poorly served in the process. The most recent example of “when they don’t” relates to the March 2016 Jakarta Naval Hospital multiplace chamber fire in which four occupants succumbed. I worked my sources in Jakarta over the ensuing months and years to no avail. There has been an information black out from responsible authorities and only unvalidated tidbits of information to be found within the lay press. Apparently, the fire occurred immediately prior to commencing ascent. The chamber was equipped with a water deluge system yet various reports stated that “the operator tried using it, but it was too late’, “the operator failed to activate the deluge system”, “the deluge system was inoperable”, and “deluge system activated but inadequate to extinguish flames”. The implications associated with each of these possibilities in the context of lessons to be learned are enormous. Without public dissemination of expert analysis, we are left to worry and wonder. The precise cause of the fire is likewise unreported. The hospital declared that “it had complied with strict operating procedures”, but I think this unlikely. A highly regarded Australian hyperbaric chamber operator colleague was inspecting another chamber elsewhere in Indonesia at a later date. He came across a technician employed by a Jakarta-based chamber manufacturer. When asked if he had any insights into the cause, the technician said nothing but knowingly pointed to his cell phone. Apparently, when the personal lockers used by the chamber’s occupants were inspected one did not contain a cell phone. This was considered highly unusual given their prevalent use. One newspaper quoted a police official as saying, “attendants might have had no courage to check whether any of them (patients) were bringing matches or cell phones in to the chamber”. This was apparently in reference to a very senior military/government official among the dead and the prevailing culture of deference. This fire had occurred at a time when one cell phone make/model’s battery had more than once generated an exothermic reaction leading to spontaneous ignition.
Clearly, much is to be gained when leaders act responsibly. When they don‘t, critical risk-mitigation measures are likely to go unaddressed or unenforced and the well-being of tomorrow’s hyperbaric patients and staff poorly served in the process. The most recent example of “when they don’t” relates to the March 2016 Jakarta Naval Hospital multiplace chamber fire in which four occupants succumbed. I worked my sources in Jakarta over the ensuing months and years to no avail. There has been an information black out from responsible authorities and only unvalidated tidbits of information to be found within the lay press. Apparently, the fire occurred immediately prior to commencing ascent. The chamber was equipped with a water deluge system yet various reports stated that “the operator tried using it, but it was too late’, “the operator failed to activate the deluge system”, “the deluge system was inoperable”, and “deluge system activated but inadequate to extinguish flames”. The implications associated with each of these possibilities in the context of lessons to be learned are enormous. Without public dissemination of expert analysis, we are left to worry and wonder. The precise cause of the fire is likewise unreported. The hospital declared that “it had complied with strict operating procedures”, but I think this unlikely. A highly regarded Australian hyperbaric chamber operator colleague was inspecting another chamber elsewhere in Indonesia at a later date. He came across a technician employed by a Jakarta-based chamber manufacturer. When asked if he had any insights into the cause, the technician said nothing but knowingly pointed to his cell phone. Apparently, when the personal lockers used by the chamber’s occupants were inspected one did not contain a cell phone. This was considered highly unusual given their prevalent use. One newspaper quoted a police official as saying, “attendants might have had no courage to check whether any of them (patients) were bringing matches or cell phones in to the chamber”. This was apparently in reference to a very senior military/government official among the dead and the prevailing culture of deference. This fire had occurred at a time when one cell phone make/model’s battery had more than once generated an exothermic reaction leading to spontaneous ignition.
A similar event occurred at Istanbul University Medical Center, Turkey, in July 1988. Fire broke out in their multiplace chamber and its three occupants, two decompression-injured divers and a physician attendant, perished. The chamber in question was circa 1947 vintage and not equipped with water deluge. Surprisingly, I received an email from the brother of the deceased physician in the days that followed, imploring me to help him determine how this tragedy could have happened. Again, the involved institution was tight lipped, and remains so more than three decades later. There is no indication that an expert investigation took place and if it did it has never seen the light of day. I have visited this institution on several occasions since and the subject of this fire is very much taboo. The best I could get was “Every professor blamed the other”.
So, what caused these fires? What aspect(s) of each institution’s fire safety plan had been violated? Or was there even an adequate fire safely plan? What, if any, attempts were made to extinguish the fire? What efforts were attempted to rapidly extricate the occupants? What critical details came to light in the immediate aftermath dealt? Sadly, we don’t know any of this, and are indeed left to worry and wonder.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2021
From time to time the NBDHMT receives requests for its position on various operational and safety issues. Our replies vary depending upon the specific nature of the question. In terms of a formal Position Statement, eleven appear on our web site which we trust you have read and remain compliant with those that relate to CHT Code of Conduct attestation. Beyond these statements, our replies will offer advice or guidance by such things as provision of a published paper, information from textbook chapters, a meeting presentation (with provision of its Abstract), an email if the answer is deemed straightforward enough, or perhaps referral to another authoritative source. Importantly, while these latter responses are intended to be helpful and consistent with our mission, they do not necessarily reflect the Board’s formal position.
We will feature example responses in these Briefings from time to time, and begin here with a common one, namely is there an appropriate/standard chamber compression rate for clinical treatments, in the context of middle ear barotrauma (MEB) risk. This is a valid enquiry. While HBO therapy is considered a mastered medical technology in the right hands, it is not complication free with MEB leading the way. Reported incidence ranges as high as 80%, although fortunately a great majority of cases are minor, don’t require treatment and will not interfere with the subsequent treatment course. Our answer is that there is no standardized rate, per se. Rather, it is very much based upon individual patient tolerance. The first compression should preferably be “slow” (in the order of 1.0 psi/2.0 fsw per minute), and may be incrementally increased with confirmation of tolerance, as directed by the hyperbaric provider. Ideally, this will include routine ear assessment (pre/post-ascent) as injury can occur in the absence of a patient’s complaint. Auto-inflation technique(s) should be taught and demonstrated, patient compliance attempts observed, preferably including otoscopic exam, during initial hyperbaric consultation. Encouraging frequent auto-inflation during compression tends to pay dividends. Patients should be observed during all pressure changes and advised to promptly report ear discomfort.
Several studies have attempted to identify ways to reduce MEB. Examples include which of three different compression rates is least injurious, 1 are scheduled pauses (compression stops) vs traditional constant rate more protective 2 and routine pre-treatment with anti-inflammatory/vasoconstrictive agents. 3 None were associated with a lowered incidence, although having compared rates of 1.0, 1.5 and 2.0 psi/min. during monoplace operations, Heyboer et al. did recommend 2.0 psi/min. 1 There was no difference in MEB between rates, (nor with respect to differing chamber treatment pressures) but as their facility uniquely starts treatment time upon leaving surface pressure rather than the more traditional start point of arrival at prescribed chamber pressure, they wished to minimize travel time in order to optimize oxygen dosing. Getting to pressure without undue delay also has value for the traditional treatment start point. It lessens contribution of oxygen uptake resulting from drawn-out compressions, particularly involving one or more forced pauses, to uptake at pressure in the context of CNS oxygen toxicity risk. It will also reduce overall chamber exposure periods in patients with degrees of confinement anxiety and improve patient turnaround times.
Dick Clarke, President
National Board of Diving & Hyperbaric Medicine
- Heyboer M, et al. Undersea Hyperbaric Med 2014;41(5)
- Ng A, et al. Undersea Hyperbaric Med 2017;44(2)
- Millian SB, et al. Undersea Hyperbaric Med 2021;48(2)
June 2021
During the recent annual directors meeting it was determined that clarification was necessary regarding correct use of NBDHMT issued credentials. What follows is that clarification and will be added to the CHT Resource Manual. Special thanks to Richard Barry for taking the lead on its development.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Use of NBDHMT Issued Credentials
NBDHMT credentials must be used correctly. Titles and credentials are registered trademarks issued to the NBDHMT by the U.S. Patent and Trademark Office. They can only be used when authorized and for a period specifically designated by the NBDHMT. In addition, guidelines exist for displaying credentials correctly. For display of proper and improper use, the Certified Hyperbaric Technologist® (CHT®) is used below but applies to all certifications issued by the NBDHMT.
Examples of correct CHT use
- John P. Doe, CHT
- John P. Doe, Certified Hyperbaric Technologist
- John P. Doe, CHT-ADMIN
- John P. Doe, Certified Hyperbaric Technologist-ADMIN
The credential may be used only for the period for which use is authorized. Use expires if renewal fees go unpaid and/or recertification requirements are not met. Use of these titles beyond the authorized period constitutes unauthorized use.
Credentials may be used on business cards, a resume, curriculum vitae, social media, and correspondence with a signature block. Credentials are awarded to individuals, not to companies or organizations, and should only be used with an individual’s name.
Example of proper company/organization use
- XXX provides advanced wound care and hyperbaric services. Employees holding the Certified Hyperbaric Technologist® (CHT®) certification include John P. Doe, CHT, and Mary P. Jones, CHRN.
Example of improper company use
- XXX provides advanced wound care and hyperbaric services by Certified Hyperbaric Technologists.
Retired Credential Holders
Individuals who retire can hold their certification in retired status should they meet the following requirements:
- Held certification a minimum of 10-years
- Completed two (2) recertification cycles
To maintain certification in retired status
- Accrue no more than 40 hours of annual operational practice
- Payment of a biannual renewal fee of $10
Individuals holding a certification in retired status must indicate their status using any of the following examples
- John P. Doe, CHT Retired
- John P. Doe, CHT (Retired)
- John P. Doe, CHT Ret.
- John P. Doe, Certified Hyperbaric Technologist (Retired)
Use of NBDHMT credentials without authority
The NBDHMT has established procedures for investigating individuals, companies and organizations who appear to be using a NBDHMT credential without authorization. The identity of anyone reporting potential violations will remain confidential.
Unauthorized use may occur online, on a business card, resume, curriculum vitae, business letterhead, brochure, or similar publication, or within a signature block.
After receiving notification of potential unauthorized use, the NBDHMT will undertake steps to determine any irregularities, which may include legal counsel.
Those who have used NBDHMT credentials without authority may be barred from pursuing NBDHMT certification for up to five (5) years. Their names may be published on the board’s website. The NBDHMT reserves the right to use the legal system to protect its trademarks.
May 2021
With immediate effect, the Board is accepting applications for a live virtual method of undertaking the 40-hour CHT preceptorship requirement. Those wishing to take advantage of this opportunity are invited to apply to the Board. In doing so, please describe how you intend to facilitate this process, including responses to the following:
- Which live virtual method (Zoom, Facetime, Microsoft Team, etc.) and device type
(phone, tablet, laptop camera) - The process(s) employed to ensure patient privacy
- Who will be the designated proctor(s)
- Student(s) name
- A timeline showing how the 40-hours will be broken into sessions, what each session will cover, and dates of the sessions. Please note that simply turning on a video camera for 40-hours and watching the student conduct chamber operations does not meet the intent of the proctorship.
Each student is still required to complete and submit the Preceptor Notification Form.
https://nbdhmt.org/forms/CHT_Preceptor_Form.pdf
This virtual preceptorship process will remain in force until formally rescinded by the Board, with 90 days’ notice. Any related questions…contact Board headquarters.
Dick Clarke, president
National Board of Diving & Hyperbaric Medical Technology
April 2021
Board sponsored diver medic refresher training this year will be via Zoom, which should not surprise anyone. In 2020, we had just managed to squeak in a live two-day face-to-face course in early March, the weekend before the country shut down. For 2021, we will run a series of four-hour sessions spread out over a couple of months. We find this easier to coordinate speakers and limit the medic’s time away from gainful employment.
The first of these sessions will take place this coming Thursday April 29, beginning at 10.00 east coast time, with four topics on tap:
- Multiplace-monoplace hyperbaric delivery systems: A comparative analysis for DCS treatment in the modern era
- Update on the contents of the diver medic’s ‘tool kit’
- Comprehensive review of the medical aspects of diver barotrauma
- Diagnosis and management of oxygen toxicity during treatment of DCI
Some 30 DMT’s are registered thus far. If you have not registered and would like to join us please fill out and email the application below to NBDHMT@aol.com or fax 866-451-7231.
Diver Medic Refresher Training Application
March 2021
Having audited a number of training course approval requests and numerous other lectures in recent years I thought it helpful to summarize several observations in the form of guidance for those of you planning to create a Power point presentation, perhaps for the first time. More experienced speakers among you may also pick up a few pointers here and there.
To begin, the preferred use of written text within a slide is to prompt a speaker’s further narrative, in the form of several bullet points for example. Too frequently, text appears as a series of entire sentences, worse still dense paragraphs. This invariably results in a speaker reading all this verbiage verbatim before moving on to the next slide and doing likewise, without offering any additional content or insight. On occasion I have wondered why the presenter even bothered to speak at all. The audience could likely do an equally effective job of reading the slides (if they were able to see them from the back of the room…next paragraph!). This approach does little to instill confidence in the speaker as a knowledgeable resource, perhaps on the contrary. When presenting on a given topic for the first time, I sometimes find it helpful to have ‘reminder’ notes visible with the Power point program in ‘Show Presenter View’ mode. As this topic is repeated to other audiences there will be a decreasing need to reference them.
Another point is the use of small font sizes to the extent that a great amount of the slide is uninhabited. Use larger font sizes so audience members don’t struggle to follow your text. When listing bullet points (preferably no more than five or six per slide) space them out to fill up the slide rather than cramping them together in one corner, thereby leaving a lot of ‘dead’ space.
If you are quoting a study, research finding or some other data, be sure to provide the audience with the appropriate reference. Among other things, this may preempt any disagreement/debate on the facts you cite, and it allows attendees to read more on the topic if it is of particular interest. Referencing can be in the form of a small text box at the bottom of the slide, the addition of a final slide that lists all the material you referenced, or perhaps a hard copy handout (available for download if the audience is virtual). Another method I tend to use is reproducing an article’s entire first page on a slide. When doing so, I occasionally highlight key messages, often within the Conclusions section. As it will often be difficult to read the citation text with this approach, I type it (minus the title which is readily viewable) in bold along the bottom of the page. In the attached link are examples of the way I tend to cite various publications, and there are no doubt others.
Something to avoid is citing material you haven’t read. In doing so, you are relying on another presenter’s interpretation of the information, which may not always be correct. To be comfortable quoting data and being able to answer related questions, a little background reading is a must. It will also serve to enhance your credibility in the eyes of the audience. If you are using images, please make sure that they are an accurate portrayal of what you are discussing. I have seen several apparent photographs of Nathaniel Henshaw, the first person to propose a hyperbaric chamber for therapeutic purposes, way back in 1664. The first photograph was not taken until some 150 years after his death. I have also seen renditions and photographs of his chamber; all attributable to other hyperbaric practitioners who arrived on the scene a couple of centuries later.
This is NOT Henshaw’s chamber.
You are very much encouraged to give talks, not the least for your own professional development. Perhaps starting out with co-workers as your audience then building up confidence to speak to larger groups is a good way to start. It will likely require a bit of background reading to become comfortable with the subject matter, but that’s a good thing in my view and worthy of committing to. Practicing a couple of times in front of co-workers, family and friends will do much to improve your confidence. It will also give you a measure of precisely how long it takes to deliver it, for scheduling and education credit application purposes. I have listened to a one-hour CEU presentation taking just 17 minutes and a 30-minute scheduled talk taking as long as 70 minutes.
Good luck!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2021
The NBDHMT is in the process of transferring responsibility for veterinary hyperbaric technologist training and certification to the Veterinary Hyperbaric Association, formerly known as the Veterinary Hyperbaric Medical Society.
With the maturing of the concert of a hyperbaric vet, in 2011, the NBDHMT was asked to serve as the administrative home for this sub-specialty designation. In agreeing to do so we invited Dr. Dennis Geiser to join the Board’s directors and charged him heading the process of formulating a training course and certification standards. Designated training subsequently became a combination of the existing human curriculum, where appropriate, with add-on sections specific to animal related safety, welfare, and clinical practice.
Over the ensuing years increasing numbers of veterinary specialists took advantage of this new professional designation. Veterinary hyperbaric interest has evolved to the point that an independent and highly focused profession accrediting organization has been introduced. All current NBDHMT certified CHT-Vs will soon notified about their lateral transfer to the VHA.
The NBDHMT wishes the VHA every success and is grateful to Dr. Geiser for his expert leadership in all of this.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2021
The Board’s administrators have asked that I make mention of the fact that restrictions that have been in place for much of 2020 have affected their ability to maintain otherwise prompt turnaround times. They seek your patience as they continue to work to the best of their abilities during this period and particularly with ongoing USPS and other mail service delivery delays. They also urge that when/if you call Board headquarters, you heed the recorded instructions and elect to either email or fax your documentation to the contacts provided (nbdhmt@aol.com or +1.866.451.7231, respectively).
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2020
December 2020
The hyperbaric industry gleans most of its safety procedures from the NFPA 99 Health Care Facilities Code (Chapter 14). Those with hypobaric chambers use NFPA 99B Standard for Hypobaric Facilities. NFPA recently published the 2021 edition of these two documents. They are available as pdfs with the view-only option at NFPA.org. Both NFPA 99 and NFPA 99B are consensus standards derived from public input. That means each of you can have direct input and impact on the codes you are required to follow. If you believe a code item might benefit from updating or a new item is needed within the code, now is your time to submit your views. June 1, 2021 is the closing date for public input. All public inputs receive committee review and comment.
The next edition is scheduled for a 2024 release. To submit a public input using the online submission system, go directly to the NFPA 99 page with these links:
NFPA 99: http://www.nfpa.org/99 and http://www.nfpa/99b
Once on the page, select the link “Submit a Public Input” to begin the process. You will be asked to sign-in or create a free online account with NFPA before using this system. If you have any questions a chat feature is available, or you can contact NFPA by email at custserv@nfpa.org or phone at 1-800-344-3555.
• • • • •
Effective January 1, 2021 those who are scheduled to retake their certification exam will be required to pay testing centers retake fees. Until now, the Board has and will continue to charge $50.00 to offset administrative time and resources required to arrange retesting. The Board then paid each center’s retake fee. This latter fee will now become the responsibility of the examinee, the amount of which ranges considerably, averaging approximately $30.00.
Dick Clarke, President (with special thanks to Richard Barry for the NFPA update)
National Board of Diving & Hyperbaric Medical Technology
November 2020
The Board’s commitment to provision of safe and effective diving and hyperbaric medicine operations extends to auditing all new applications for course approval. Board members regularly volunteer their time without compensation or expectation to ensure that faculty members for these courses possess requisite knowledge and teaching skills and that educational materials are appropriate and reflective of current standards. The recent advent of virtual teaching via Zoom-like platforms due to the COVID-19 pandemic has added to this audit case load as previously approved face to face programs require spot checks to address adequacy in this new format. I’m actually helping with one of these as I write this month’s Briefing.
But these audits do have their lighter side and the good Dr. Henshaw frequently features. You will likely recall that it was he who first proposed an alteration in atmospheric pressure for therapeutic purposes, in his 1664 publication “Aero-Chalimos or, a Register for the Airs”. In one well-intended lecture referencing this pioneering concept, there is an accompanying photograph of Dr. Henshaw looking everything the respectable academic. The issue here was that he had died a little more than 150 years prior to the first photograph being taken, circa 1826. On another occasion, an artist’s impression of Henshaw’s “Domicilium” is included on the slide. What is actually depicted is Fontaine’s mobile (horse drawn) hyperbaric operating room, again developed more than 150 years later. Although Henshaw described his chamber/Domicilium he did not include any image in his publication, so readers are left to conceptualize what it may have looked like from its detailed operating characteristics. During one other talk, Henshaw is glowingly referenced as the father of hyperbaric oxygen therapy. Nowhere in Henshaw’s publication is oxygen referenced. This is hardly surprising as it would be another 100 years before the gas that would eventually be called oxygen was discovered. One presenter’s slide referenced Dr. Hank Henshaw. His mother may have been somewhat distressed to learn that her dear son Nathaniel had had his name so contracted.
To conclude from my Monthly Briefing soapbox, I would now wager that despite long-standing dogma, Henshaw was not the first to use a hyperbaric chamber. There were just too many flaws in his proposed design and operating principals. But that is a story for another day.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2020
While auditing an introductory hyperbaric training course the other day I heard mention on several occasions that the humidity level within the monoplace was always zero. This statement served to justify a requirement that patients should remove their contact lenses before each treatment. The stated basis for zero humidity was that incoming LOX sourced oxygen was dry.
This statement failed to account for the patient’s ongoing respiratory and transcutaneous evaporative insensible moisture loss. Historically, our group had measured monoplace chamber relative humidity under varying conditions, namely changes in oxygen flow rates and differing patient body mass. RH was never zero, rather it was found to range from the low 20’s to the high 60’s. The lower the flow rate the higher the resulting RH. Experienced chamber operators may have observed RH levels so high on occasion that condensation occurred on the internal surfaces of the acrylic hull.
From a monoplace chamber fire safety perspective, one should aim for the higher of the above range. Dryer conditions tend to result in a higher risk of static electricity buildup, which can lead to dangerous electrostatic discharges if patients are not appropriately grounded. If patients complain of being cold while in the chamber this should prompt a reduction in oxygen flow, not provision of a (another) blanket! The 1996 monoplace chamber fire and explosion was an object lesson, in that combustible materials must be limited to the greatest extent possible. If patients complain of being too warm, titrate the oxygen flow higher. Do not simply default to the highest flow rate…comfort levels may be reached with only incremental increases.
I thought it useful to revisit this topic. Too commonly, oxygen flow is maintained at its highest rate, as a previous patient may have complained of overheating. When subsequent patients become too cold the default position may be to provide an additional blanket, or two. Consistent with the above, this would be considered F work! Don’t do it.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2020
Recently, the Baromedical Nurses Association Certification Board introduced a revised continuing education log (see below). It is to be used to record all related activities and submitted during the CHRN recertification process. It has been added to the NBDHMT website and can be found within the ‘Hyperbaric Nurses’ link.
The BNACB also notes that in order to receive discounted certification and recertification pricing, nurses must provide proof of either BNA, UHMS or ACHM membership at the time of application. Discounted certification rates are $250.00 for BNA membership and $300.00 for UHMS/ACHM membership. Recertification rates are $150.00 and $200.00, respectively.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology.
https://nbdhmt.org/forms/CHRN_CE_Log.pdf
https://nbdhmt.org/forms/CHRN_Exam_Registration_Application.pdf
https://nbdhmt.org/forms/CHRN_Recertification_Application.pdf
August 2020
I had rather a lot going on last month so failed to allocate time get my regular briefing published, regrettably. What I thought I would do is fill that month’s space with one of my recent blog posts. Readers may find the various methods that have been considered to blind study patients during the (all too few) sham controlled clinical trials to be of particular interest.
Patient Blinding During Hyperbaric Trials is Possible and Essential
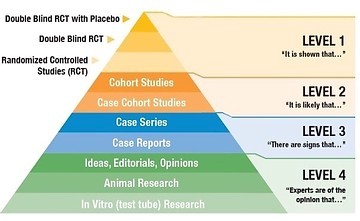
The Evidence-Based Medicine Hierarchy
Pioneering cardiac surgery within a pressurized chamber heralded the modern era of hyperbaric medicine. While the almost immediate introduction of cardiopulmonary bypass technology proved hyperbaric surgery short-lived, its hyper-oxygenation mechanism was adopted to treat several other acute ischemic states. Identification of additional therapeutic mechanisms associated with hyperbaric hyperoxia led to its use elsewhere, with hyperbaric medicine emerging as accepted practice despite a paucity of robust supportive evidence. That its early proponents included highly regarded academicians may well have played an influencing role.
The advent of evidence-based medicine (EBM) has changed the medical practice calculus. There is increasing expectation that therapeutic interventions be proven efficacious, safe and cost-effective. While this applies to medicine in general, the continued failure to produce convincing data in support of its common indications finds hyperbaric oxygen (HBO) therapy firmly beneath the evidence ‘microscope’. Within the United Kingdom for example, once at the forefront of hyperbaric research and clinical activity, the National Health Service, the UK’s principal underwriter of health care, has whittled down reimbursement to a single condition, decompression sickness. All previously approved uses have been delisted.
Need for better data
While the UK example is extreme, frustration regarding evidence shortcomings is widely apparent elsewhere. Ready acceptance of negative studies otherwise noted to suffer patient selection, study design, protocol compliance, and data interpretation flaws (Scheinkestel et al. 1999; Annane et al. 2002; Fedorko et al. 2016; Glover et al. 2016 as examples) has clearly influenced policy makers, authoritative practice guidelines, meta-analyses, invited editorials, and others who purchase healthcare. With few exceptions, there has been a failure to undertake well designed and executed randomized sham-controlled double-blind trials. As noted in the accompanying evidence hierarchy diagram, this study type is considered the highest level and most reliable form of research methodology. In its absence, hyperbaric medicine will continue its struggle for broad acceptance within ‘mainstream’ medicine.
Sham vs placebo
You are likely more familiar with the term placebo, which is defined as an entirely inert substitute to active therapy. Placebo studies are common during new drug investigations, with the inactive agent often referred to as a sugar pill. One cannot employ placebo during hyperbaric research, although some studies have incorrectly used this term. As patients are required to enter a chamber rather than swallow a pill, they will be exposed to incidental and potentially harmful effects. During the 2010 Londahl et al. DFU trial for example, one sham (which the authors termed placebo) patient fell while in the chamber suffering a head injury requiring hospitalization. Several sham patients experienced ear barotrauma, necessitating surgical intervention (needle myringotomy) in two patients, and four others suffered hypoglycemia: all hardly representing inert blinding.
Sham studies are those in which blinding is required during investigation of a procedure or intervention. As one cannot feign entering a chamber, one must simulate aspects associated with it. Sham is defined, therefore, as a fake procedure that omits the step thought to be therapeutically necessary. Sham patients should ideally, therefore, experience the incidental effects of chamber exposure absent hyperoxia (active therapy).
How can sham exposures be undertaken?
Several methods have been employed.
- Air breathing compression to equivalent pressure of the active treatment group, thereby exposing sham patients to compression/barotrauma issues and chamber warming/cooling. Its drawback is that patients will experience elevated oxygen tensions (Dalton’s Law), thereby confounding assessment of magnitude of any oxygen effect between groups. There is also a risk of decompression sickness, the degree of which being dependent upon chamber pressure/duration. Attempts to mitigate this risk with oxygen breathing during slowed decompression may result in unblinding.
- Air breathing compression to equivalent pressure of the active treatment group, then switching from air to a percentage of oxygen, balance nitrogen, equal to that of normal atmospheric pressure (examples: 7% at 3.0 ATA – 8.75% at 2.4 ATA – 10.5% at 2.0 ATA).This serves to eliminate the elevated oxygen issue but increases risk of decompression sickness. It also adds a degree of technical complexity.
- Maintaining sham patients within an unpressurized chamber while breathing air. The shortcoming of this approach is that incidental effects are absent. This would become all too readily apparent having undergone the informed consent process (where such effects are described) and should patients from each group encounter one another.
- Air breathing compression to an intermediate pressure (commonly 1.34 ATA) in order to produce incidental effects, then immediate gradual decompression to normal atmospheric pressure for the remainder of the planned exposure period. This approach has been statistically validated as an effective blinding technique (Clarke, at al. 2008; Weaver et al. 2002), and recommended for subsequent trials. It also serves to eliminate decompression sickness risk, as it does the confounding elevated oxygen pressure exposure.
In summary:
- A validated method exists to effectively blind patients during hyperbaric trials, and
- Randomized sham controlled double blind trials are the ‘proof of evidence’ gold standard and required to fully validate HBO therapy in this modern era
This current lack of efficacy evidence does not mean lack of clinical effectiveness if appropriate research is yet to be undertaken. It does mean that proof of evidence studies are essential for the continued availability and viability of HBO therapy, in order that select patients continue to gain access and benefit.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2020
In response to the COVID-19 public health emergency, the Board has approved livestreaming of introductory courses in hyperbaric medicine. This is a departure from the Board’s long-standing position that such training be delivered in a face-to-face setting. This decision has been conveyed to Board-approved instructors, noting an effective date of July 1. The live-streaming option will be in effect for as long as the public health emergency remains. Details on precisely how livestreaming is to be conducted and attendance verified can be viewed in the link below.
Livestream Course Approval (PDF)
If you have any questions related to this change please contact Board headquarters at nbdhmt@aol.com
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2020
Continuing education is mandatory for health care professionals and hyperbaric team members are no exception. Among other things, it affords exposure to new information, consolidates existing knowledge and introduces evolving standards. It is anticipated that the sum of all of this is maintenance of best patient care and related safety.
The Board receives a wide range of continuing education requests and approves those deemed consistent with the above criteria. Awarding of credits commonly results from attendance at meetings, conferences and training courses, employer-based learning opportunities and various online initiatives. In the context of the CHT, the Board considers hyperbaric delivery system operations, its related technical aspects and chamber safety to represent core competency. Accordingly, these topics should represent the primary focus of a CHTs continuing education. Consistent with this position, the Board requires that a minimum of nine of the minimum twelve 12 Category A credits directly address these topics.
Re-certification requests occasionally fail to meet this requirement and applicants notified to undergo increased core competency updating prior to re-submission. This is common with CEU exposure to more generalized material. Examples include review of existing and proposed hyperbaric indications, related pathophysiology, claims filing and reimbursement nuances, clinical practice updates more suited to providers, and other “peripheral” medical topics. In order that the CHT maximizes their value equation (quality and appropriateness of continuing education over its cost of acquisition), the Board now requires the following statement to accompany all subsequent references to NBDHMT approved CEU, one that serves as a reminder of CHT core competency:
“CHT re-certification requires a minimum of nine of the minimum 12 Category A credits relate directly to any combination of hyperbaric operations, related technical aspects and chamber safety”.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2020
The COVID-19 pandemic continues to hold the world’s attention. Governments and leading health policy organizations have provided largely consistent guidance on how best to protect oneself from becoming infected and otherwise limit potential for disease transmission. The closed environment of the hyperbaric chamber represents a unique challenge in this regard, particularly as it relates to multiplace chamber operations.
Authoritative undersea and hyperbaric medicine societies have issued safety and operational guidelines to mitigate against possible contagion within patients and staff members. While they vary in extent and specifics, they convey a broadly consistent message. Each is worthy of your review, regardless of geographic affiliation, and are accessible via the links below. Three of these organizations caution against HBO as treatment for COVID’s viral effects and associated hypoxia. The Canadian document does add that anyone contemplating such use should only do so following Institutional Review Board/ Ethics Committee approval.
A very small and uncontrolled report from China suggests HBO’s benefit with no apparent adverse events. I am familiar with eight formal studies intended to address HBO’s therapeutic potential, each presently undergoing, or about to undergo, IRB review. Four are in the US (two New Orleans, one New York, one Cleveland), one each in Canada, Sweden, France and Italy. Full details of three are viewable at www.clinicaltrials.gov ID’s NCT04327505, NCT04344431 and NCT04332081. There is little consistency within these studies regarding hyperbaric dosing pressure, duration, frequency and course. This has both advantages and disadvantages.
Long-standing Board member Dr. Keith Van Meter deserves a special shout out in all of this. Those of you who know him well enough will appreciate his one constant is unselfish expert support of many things diving and hyperbaric medicine. He never seeks and invariably avoids the limelight. The two New Orleans studies are further examples. Behind the scenes, he has put a great deal of personal time, personal finances and other key resources to get these studies up and running. Thank you yet again, Keith.
Until next month’s briefing stay safe and well.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Addendum to the CUHMA Guidelines for Hyperbaric Medicine: COVID-19 pandemic
April 2020
That Other Pandemic and the Birth of Hyperbaric Oxygenation
The current pandemic brings to mind that last great pandemic (1918-1920) and the actions of one physician who became the first to employ a hyperbaric chamber specifically to drive additional oxygen into tissues. Today we call this process hyperbaric oxygen (HBO) therapy and its first patients were Spanish Influenza victims.
 Orval J. Cunningham 1880-1937 |
Early Hyperbaric Chamber Use
Until this period, the singular therapeutic basis for hyperbaric chamber use was that of the inverse relationship between pressure and volume, namely Boyle’s Law. Workers exposed to compressed air during bridge construction and mass transit tunneling projects were at risk for “caisson disease”, now referred as decompression sickness. This condition resulted from formation of embolic gas secondary to inadequate decompression. Re-exposing injured workers to elevated air pressures within a hyperbaric chamber reduced/eliminated offending gas, frequently affecting cure. By the turn of the 20th century, “recompression” chambers were increasingly commonplace at civil engineering worksites incorporating compressed air. Naval and civilian divers, likewise at risk of decompression sickness, were soon to benefit in a similar manner.
Oxygen as Therapy
The discovery of oxygen occurred some 150 years earlier. However, it had remained more of a research curiosity until 1922 and the publication of Haldane’s seminal work “Respiration” before it finally entered mainstream medical therapeutics. Although Haldane proposed its clinical use several years earlier, “Respiration” clearly got everyone’s attention. Unfortunately, the outbreak of Spanish Influenza pre-dated this advancement, leaving its victims struggling to breathe with nothing more forthcoming than the oxygen concentration in normal atmospheric air. For a great many this proved woefully inadequate.
HBO’s First Patients
Enter Orval J. Cunningham, Associate Professor of Surgery and Chair of the Department of Anesthesia at the University of Kansas Medical Center. Cunningham was considered a remarkably keen clinical observer. In one example, he had noted that patients with lung diseases appeared to improve when traveling from Colorado to Kansas. Another example, and more critical at the time, was that the pandemic’s morbidity and mortality was greater in areas of high elevation, such as Colorado, compared to coastal regions. As an anesthesiologist, Cunningham was understanding of Dalton’s Law and its effect on gas pressures. He rightly considered that the only significant variable was an increase in oxygen pressure as altitude decreased. He sought to determine if further increases in ambient air pressure beyond normal atmospheric pressure could produce a clinically meaningful effect. To investigate this he borrowed a small hyperbaric chamber from a local diving contractor and arranged for its installation at the university medical center. In it, he treated several profoundly cyanotic and moribund influenza patients and met with “instant success”. “Patients whose lips bore the blue-black livid stamp of the kiss of death and were deeply unconscious, but if not too far from the brink, in a matter of minutes were brought back to normal color and return to consciousness”. Importantly, Cunningham had no access to oxygen. He had managed to accomplish these marked clinical improvements by the simple act of increasing chamber pressure with air, letting Dalton’s Law do the rest. History should acknowledge, then, Dr. Orval J. Cunningham as the first hyperbaric oxygen practitioner. It would be another 15 years before oxygen breathing under hyperbaric conditions was introduced, thereby forming the basis for the modern practice of hyperbaric medicine.
By late 1918, the second and more deadly wave of the pandemic had started to subside, so too the number of its victims treated by Cunningham. With additional and much larger chambers under consideration and a diminishing influenza caseload, he sought out other conditions that he thought might benefit from increased oxygen delivery afforded by elevated air pressure. This journey eventually resulted in him condemned by the American Medical Association and his legacy forever tarnished.
Oxygenation of Today’s Pandemic Victims
Fortunately, today’s influenza sufferers have ready access to unlimited supplies of oxygen. Delivered at normal atmospheric pressure within the ED and ICU, it results in higher doses than those achievable within Cunningham’s compressed air chamber. Mechanical ventilation, when indicated, further enhances oxygen’s therapeutic effect.
References available upon request.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2020
 Terrence E. Overland |
The commercial diving community lost a stalwart and friend with the passing of Terry Overland on February 19, at age 71.
Terry’s journey to the upper reaches of diving industry health and safety began upon separation from the US Navy, in 1974, and subsequent completion of commercial diver training. He worked his way from the professional diver’s lowest rung, tender, to eventual leadership positions within the world’s largest diving companies. I first met Terry in 1977. He attended one of our early diver medic training courses sponsored by UCLA Medical Center and Commercial Diving Center. He was a focused and motivated student, asked many good questions, and clearly determined to put his medical training to good use; that he certainly did.
Terry joined the NBDHMT as a director in the early 1990’s. He served unselfishly and to good effect, representing a key link between the Board and the commercial diving industry. He regularly and readily gave up his personal time without hesitation or expectation to help teach the Board’s diver medic refresher courses.
Terry had only quite recently begun a well-deserved retirement. He relocated to Florida and a nice little property overlooking a pristine beach bordering the Gulf of Mexico. He would occasionally email me a photo of him sitting on his deck in the early morning sun, feet up and coffee mug in hand, cheekily asking how my morning was starting out! Sadly, his retirement was much too short. Importantly, however, his contributions left behind a safer diving industry than the one he found. Many of today’s working divers are unlikely to have met or even heard of Terry but will surely benefit because of him if they suffer a decompression injury. Terry’s bio can be read at this link. https://www.nbdhmt.org/overland.asp I wanted to add a brief perspective of our 44-year professional and personal time together.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2020
The Baromedical Nurses Association Certification Board have created an updated version of their CHRN Hyperbaric Service Log. The initial version was a little “wanting”; we had received several requests to produce a more intuitive version. This has since occurred and accompanied by helpful instructions on how to complete and submit it.
https://nbdhmt.org/forms/CHRN_Experience_Log.pdf
We found it necessary to cancel the annual DMT refresher-training course for the first time since introduced back in 2012. There were insufficient registrants to warrant the costs of hosting it in New Orleans. Several medics expressed disappointment as they badly needed invasive skills updating, among other things. To accommodate their request we decided to run a two-day refresher here in Columbia, March 6/7. Registration is free and 16 have signed up thus far. If this interests you, contact Board headquarters ASAP. The course outline viewable here.
https://nbdhmt.org/forms/Columbia_DMT_Refresher_Agenda.pdf
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2020
Happy New Decade!
It was 11 years ago this month that I began generating these Briefings, and coincided with my reassuming the role of Board president. Their intent has been to keep you up in touch with Board activities and other mission related topics that may be of interest. I have managed to come up with something over the years. However, I would certainly welcome addressing any suggestions you may have.
By my count, then, here comes number 133.
A reminder to you diver medics that the annual DMT refresher course will take place on February 5-6, and again in the ‘Big Easy’, AKA New Orleans. This is an excellent opportunity to acquire necessary recertification credits and acquire all-important hands-on comprehensive invasive skills re-training. You are encouraged to email in to the Board any questions you may have related to diving medicine and your medic role. Expert faculty members will address them during the various presentations.
https://www.nbdhmt.org/forms/DMT_Refresher_Training_Application_2020.pdf
CHT/CHT-V’s, please be reminded that nine hours (so 75%) of Category A recertification credits should be related directly to what your role involves; namely chamber delivery system operations and related safety. It is perfectly acceptable to gain credits related to clinical and other aspects of diving and hyperbaric medicine, and they can certainly ‘spillover’ the 12 Cat A credit minimum. However, key to knowledge and skill retention/ updating is ongoing exposure to those topics that serve to assure safe and effective delivery of hyperbaric medicine. Seek advice from the Board if you have any difficulty locating suitable credit sources.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2019
December 2019
As another year and another decade draws to a close I was reflecting back on the history of the Board’s certification programs while jogging along the canal on a chilly (South Carolina chilly that is) Sunday afternoon.
Commercial Diving Center, Wilmington, California, hosted the first diver medic course back in 1975. The Board was formed and DMT certification introduced several years later, as we finally gave up on encouraging the National Registry of EMT’s to adopt a DMT category of medical first responder. The people at the Registry could never warm to the reality that a DMT might be practicing several hundred miles from a medical facility and several days from surfacing from a saturation treatment, before patient transport could even begin! To date, 2,665 diver medics have certified through the Board. The first CHT examination took place in San Diego, in 1991, with some 75 testing, including many of the hyperbaric technical ‘luminaries’ of the day. As of this month, there are 4,529 CHT’s. The CHRN program followed in 1996 and 1,321 RN’s have since certified. Next up was certification in veterinary hyperbaric technology, beginning in 2011. To date 35 veterinarians and veterinary techs have certified.
For the current calendar year, 52 diver medics, 33 RN’s and 88 techs have undergone certification testing. They have done so from across the US, and within Canada, Saudi Arabia, Hong Kong and Malaysia. Overall, the first attempt pass rate was 74%. Eleven other individuals will test during the remainder of this month.
I will close by again expressing my gratitude to the Board’s directors and headquarters administrative staff for another successful year in support of diving and hyperbaric operational safety and quality.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2019
The Board recently forwarded a Canadian Government alert regarding the use of “soft-shelled” hyperbaric chambers (link below). In this notice, Health Canada makes it clear that these products are unauthorized medical devices. Companies that manufacture and sell them are instructed to immediately stop doing so and conduct a recall. Any further importation is now banned.
The basis for this chamber design is the Gamow (“Gamoff”) bag, a single person inflatable device introduced in the 1980’s. The Federal Drug Administration (FDA) approved it to treat serious cases of altitude sickness, including high-altitude cerebral edema and high-altitude pulmonary edema. Being lightweight and transportable, it allows such treatment to begin while patients remain at altitude. When “foot pump” compressed with air the device has the physiologic effect of decreasing altitude/increasing oxygen delivery, thereby facilitating recovery.
A number of companies have produced Gamow bag variants for lay populations to acquire and install in their home. They are also marketed to health spas and various other non-mainstream medical settings. Manufactures market them for an extensive range of illnesses and diseases, none approved by the FDA. It is these unsubstantiated claims, and associated risks, that is at the heart of the Health Canada alert.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2019
Some of you may recall a request we made back in 2014 for assistance with a research project involving Gulf of Mexico diving operations. A number of diver medics subsequently helped with a Doppler Monitoring Study. The organization involved has continued to study Doppler detection of venous gas as a surrogate for decompression stress, in both real-time operations and with stored datasets. A recent publication addressed the latter. Interestingly, it found that subclavian site bubble detection correlated more favorably with DCS incidence than the more traditional precordial approach. (See link below)
I have invited this organization to make a presentation at the February 2020 DMT Refresher Training Course. They are keen to continue to get access commercial diving operations and hopeful of contacts with those in attendance and elsewhere at Underwater Intervention. Among other things, they have created a self-measurement Doppler Monitoring System. The diver assesses subclavian vein blood flow, with the recording stored on a smartphone and transmitted to the organization’s server once the phone connects to Wi-Fi or a cellular network. Within minutes, the diver receives a graph assessing how optimal their decompression was.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
https://www.dhmjournal.com/images/ImmediateRelease/Hugon_Subclavian-VGE-scores.pdf
September 2019
An early head’s up for diver medics in need of invasive skills practice and continuing education credits. We have scheduled the next DMT Refresher Course for February 5 & 6. It again coincides with “Underwater Intervention”, at The Ernest N. Morial Convention Center, New Orleans. If you wish to attend this refresher opportunity, please register at https://www.nbdhmt.org/forms/DMT_Refresher_Training_Application_2020.pdf.
In addition, if there are any topics you would like to have included send please them over to Board headquarters. We will do our best to get all of your requests included in the program. The same applies to any questions you would like the speakers to address.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2019
The Board reached something of a milestone this month with the awarding of CHT certificate number 4,500. This impressive number has been achieved over a 28 year period, the first certificate being awarded in October 1991.
Online testing at accredited centers in the U.S. and overseas continues to account for all new applicants, with a test frequency averaging every other day. This process has served to streamline testing and eliminate the potential for exams to fall into the wrong hands. One such breach earlier in this decade required an extensive and time consuming re-write of much of the question test bank. All is much more secure today.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2019
I would be remiss if I failed to recognize the enormous contributions Dr. Keith Van Meter has made to the successful longevity of the National Board. Keith has served as a Board Member for the past 20 years, the first decade of which he generously housed our administrative headquarters within his business office, in New Orleans, AKA ‘The Big Easy’.
Keith represents a key medical and professional link between the Board and the environment of the working diver. Amongst other things, Keith has gone to great lengths to ensure the viability and validity of the diver medic program, and on an international scale. He has done so readily and always without expectation. Some of you may unaware that Keith is arguably the most experienced and capable of diving medicine specialists. He has readily, and frequently, put his personable well-being on the line to enter the medically and geographically remote deep diving support systems. Under some of the most challenging and stressful of conditions, he has literally saved lives and salvaged acutely damaged central nervous systems.
A ‘thank you Keith’ barely seems adequate for all he has done, but it is likely more that he would expect.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2019
The Board enjoys a long history as a trusted and respected resource. We frequently answer questions addressing operational, safety and technical aspects of undersea medicine and hyperbaric oxygen therapy. When appropriate, supportive literature and documents are provided to augment responses. The Board has generated a number of Position Statements that address key issues, and appear on our website.
What the Board is not able to do is address questions and provide advice related to medical practice, particularly with regard to ongoing clinical situations. This is beyond the scope of the Board’s mission and its core competency. Callers are advised of this limitation, sometimes to their frustration, but we hope that they eventually respect our position. Depending on the precise nature of a question, callers are invariably referred to one or more alternative resources.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2019
The Board frequently receives requests to award continuing education credits for various educational activities. Each request is analyzed for content, speaker(s) qualities and duration. The number of credit hours and credit type are then determined. Sponsoring organizations who are awarded credits are encouraged to announce this within their promotional materials.
If you are considering registration for an activity that does not carry NBDHMT credits contact the activity director. They may have failed to post this information. They may have also neglected to apply and your prompting may encourage them to do so. You can contact the Board, where a record of all approved activities is maintained.
I wanted to run through all of this because the Board occasionally receives a call from someone who attended a program and had hoped to use its hours towards recertification, only to learn that no credits were awarded. Save yourself this angst and a potential costly outlay by checking first.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2019
A few moments spent clarifying certain terminology should prove helpful to instructors, hyperbaric team members and prospective CHT/CHRN’s, alike.
It has become all too common to refer to “dive tables”. As common as it is, there are no “dive tables”, per se. Moreover, this term is used interchangeably from time to time when referencing both decompression tables and decompression illness (DCS & CAGE) treatment tables. A recent CHT examinee complained that “dive tables 5 and 6” were not in her test package. “Treatment Tables” 5 and 6 have never been part of that package. While examinees do need a fundamental understanding of clinical indications for Treatment Tables 5 and 6, there is no requirement to access these tables during the testing process. On the contrary, questions related to ascent procedures from compressed air exposures do require calculation, with decompression tables provided.
Going forward then, and to improve both clarity of intent and minimize confusion, get into the habit of using the following terminology;
- When referring to the process of calculating diver decompression obligations, its “decompression tables”. While there are several recreational diver organization variants, prevailing tables in the U.S. are those of the U.S. Navy, so “U.S. Navy Air Decompression Tables” (when air is the breathing medium) would be the full title, although “decompression tables” will commonly suffice. As an aside, many of the world’s navies have established their own decompression tables, so international colleagues may use their country’s prevailing procedures.
- When referring to the management of decompression illness, it’s “treatment tables”. Here in the U.S. and commonplace internationally is employment of “U.S. Navy Treatment Tables, 5, 6, 6A and 9.
Avoid using the term “dive tables”, and never use it interchangeably when referring to computation of decompression obligations and management of decompression illness.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2019
A note to multiplace chamber personnel regarding inside attendant decompression sickness risk mitigation when using US Navy Treatment Tables.
It has been the navy’s goal to eliminate tender DCS. They have attempted to do so by incrementally increasing isobaric oxygen breathing periods with essentially every revision of USN Diving Manual, and they appear to have been successful. In reply to a Freedom of Information Act request, the navy reported zero cases involving Tables 5, 6 and 6A from 2006-2016. In order to emulate this enviable record within the civilian sector, it is important to adopt the navy’s oxygen decompression procedures in their entirety. This includes accommodations for table extensions, beyond one, for any hyperbaric exposure within the previous 18 hours, and while operating at altitude (2,500 feet and higher). Altitude “correction” factors are not published within the standard decompression guidance on each table, but can be found in Chapter 17, Table 17-7 of the current Manual (Revision 7, December 1, 2016). The two nurse tender decompression fatalities both involved support of injured divers on US Navy Treatment Table 6A. They would have likely benefited from today’s decompression standards, particularly in the case that happened to represent a repetitive ‘dive’, which now mandates an additional 60 minutes of oxygen breathing.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2019
Effective 2019, all certification exams will be administered via online testing at recognized testing centers. The Board has been evolving to this standard in recent years. During 2017-2018, 90% of all tests were already being conducted in this manner. This process ensures the highest possibly integrity and also allows immediate availability of exam results.
Prompting evolution away from paper tests were two instances in which the designated preceptor violated their responsibility to keep individual hard copy exams secure. In one instance, the breech appeared significant enough to warrant a re-write of many of the examination bank questions.
Many thanks to all of you who have served as preceptors over the past two decades.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2019
I know that you have all been anxiously awaiting a January briefing!
For several years, the Board has awarded CEU’s for manufacturer-based transcutaneous oximetry training. The basis for this was the introduction of a requirement that prospective CHTs and CHRNs undergo such training as a certification prerequisite. When the Board first mandated this not all approved hyperbaric training programs incorporated transcutaneous oxygen testing. This meant that the equipment manufacturer was able to fill an important knowledge and testing gap.
Eventually, every program applying for or seeking to renew Board approval was required to have this important screening technology incorporated within their core curriculum. Today, this is universally the case. Therefore, associated credits will have been earned upon successful completion of introductory training. The required hands on practical requirement of at least three studies must be overseen by someone with clinical background. This can be a member of the physician panel, a vascular technologist, CHT/CHRN, or other clinically-based individual with appropriate experience.
Going forward, then, the Board will no longer be awarding CEU’s for manufacturer provided training. The Board does wish to extend its gratitude to those manufacturers who had stepped in to help a great many hyperbaric team members who would have previously had a difficult time meeting this certification prerequisite.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2018
December 2018
Fatal chamber fires are utterly devastating events. If anything good can come of them, however, it is a comprehensive root cause analysis. In this way, factors that led to the fire allow the hyperbaric discipline to fine tune existing, or develop new, policies and procedures to mitigate against similar operational failures. It is factors, not factor. Almost without exception, a sequence of events will have led to a fire. It is doubly tragic, therefore, when the results of such an analysis remain unpublished.
This is precisely what has occurred with the 2016 Jakarta, Indonesia fire. All four occupants of one of the naval hospital chambers succumbed. This fire raised several questions, none answered, at least in the public forum. I have a physician friend and colleague who works in Jakarta. As much as he tried, he was unable to obtain a copy of any form of formal documentation relating to the circumstances surrounding the fire. Again, this is very unfortunate and very irresponsible. As difficult as it to acknowledge failings that may prove embarrassing, all future hyperbaric chamber occupants deserve access to this information. Interestingly, I did receive some unofficial insight in recent weeks. The source was an engineer associated with the chamber’s manufacturer. While not authorized to discuss the events surrounding this fire, he did confide that one of the patients, a very senior military officer, had apparently taken a cell phone into the chamber. This appeared to be the ignition source. Why the installed deluge system was not activated is also publicaly unknown. One local newspaper had reported, “It was too late to use it”. We can take that statement for what it’s worth.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2018
At the annual Board of Directors meeting earlier this year, Board members decided to introduce a series of DMT invasive skills updating opportunities. The injured diver depends on the ability of the diver medic to perform these skills in the medical and geographical setting, and they are somewhat perishable if not maintained. Diver medics have consistently complained of the lack of such opportunities. In recent months, the Board purchased a range of manikins and related supplied. Contacts with several experienced paramedic instructors in various regions. They have agreed to teach these skills labs with Board provided equipment. They will receive a stipend and all related expenses underwritten by the Board. There will be no cost to DMT’s or their employers. The first such course took place at Divers Institute of Technology, in Seattle, earlier this month. Two groups attended over two consecutive days. A course has been scheduled for some 30 medics at NASA’s Sonny Carter Training Facility, in Houston, in January. Several other locations are in the planning stages.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2018
The next annual DMT refresher training course has been scheduled for February 6 & 7, 2019. As in the past, we coordinate this with the annual Association of Diving Contractors International meeting in New Orleans.
An advisory email went out to all DMT’s several weeks ago. Expressions of interest were numerous so if you are planning to register please do so in the near future. While classroom size is essentially unlimited for the didactic sessions, we do have to limit attendance due to the invasive skills sessions. For additional information, please go to the following link DMT Refresher Training 2019 Application.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2018
The Board welcomes Jay Duchnick as its newest Board Member. Jay replaces Bill Gearhart who rotated off the Board after a helpful and supportive 12 year stint.
Jay serves as program director at the Hyperbaric Medicine Center at UC San Diego Medical Center, a position he has held for more than two decades. Prior to joining this prestigious program, he spent six years as an Oceanfront Lifeguard and eight years as an aviation survivalman and helicopter rescue swimmer in the U.S. Coast Guard. Jay is an RN and a CHT. He has a number of Abstract presentations to his credit and is co-author of two peer reviewed scientific publications. Most recently, Jay has volunteered as an NBDHMT on-site auditor for new training course applications.
We are delighted to integrate Jay’s knowledge and skill into the Board’s mission.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2018
I am pleased to welcome Peter Goodman as our newest Board Member. Peter replaces long-standing member Terry Overland. Terry has retired to his home and front porch overlooking the Gulf of Mexico after a four decade history of commercial diving leadership. We would not let Terry leave the Board until he had found a suitable replacement, and in Peter he did.
Peter has an equally impressive offshore commercial diving resume. It extends almost 40 years, the last 20 of which have included diving medicine issues. His roles include health, safety and environmental, diving operations, compliance and management. Peter has some 20 certifications that represent the continuum of the diving operations and safety work place, and he has worked on a worldwide basis.
Peter will continue to ensure a close professional affiliation exists between the geographic and medically remote diver medic and the NBDHMT.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2018
A note to advise of several personnel changes taking place within the Baromedical Nursing Association Certification Board.
Debbie Critz has recently completed her six year term, the last two as the Board’s Chair. We express our appreciation and gratitude for her stewardship of the BNACB during this period. Moving up to replace Debbie as Chair is David Beavers. David is a retired US Air Force nurse. He lives in San Antonio where he is employed as a diabetic educator.
Joining the BNACB as its new member is Angela Savage, who along with Debbie Gonzalez, makes up a three person team.
As we welcome Angela, we also look forward to continuing a close professional relationship in service of the hyperbaric nursing profession.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2018
The Board concluded its annual meeting on June 29. As is common, we meet in conjunction with the Undersea and Hyperbaric Medical Society and their annual meeting. This allows our Board Members who plan to attend the UHMS meeting to be more cost efficient.
This year’s meeting saw the final attendance of Terry Overland. Terry has been a member for more than two decades. During this time, he has been a key link between the Board and the commercial diving industry, where he spent his career. Terry retired several years ago but stayed with the Board until this past month. The Board owes Terry an enormous debt of gratitude. He worked tirelessly and without expectation to improve the health and well-being of injured divers through support and promotion of the DMT training and recertification program. Thank you Terry O!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2018
Diver medics frequently have difficulty maintaining their invasive skills capabilities, skills that can prove critical in the medical and geographic remoteness of the professional diver’s workplace. In an effort to help overcome this shortcoming, the Board has introduced a one-day skills updating program. It will take place at the location of various companies who employ DMT’s, and at no cost to them. The Board will underwrite all related expenses, which will include provision of manikins, a paramedic instructor/trainer and a set of teaching Power points for each respective skill.
The program will begin in the fall. If you are a DMT, please advise your employer and put them in touch with Board headquarters for further details.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2018
 Dr. Dean Heimbach |
It is always sad to learn of the passing of a leader in our field, and the death of Dr. Dean Heimbach last month is certainly no exception. Dr. Heimbach enjoyed a long and distinguished career in both military and civilian hyperbaric medicine. Importantly for our organization, Dr. Heimbach served for many years as the Board’s ‘Public Advocacy Member’. In this capacity, he would help ensure compliance with our mission and purpose, he would make sure that the Board had adequate resources to be up to its mission, and he would provide some oversight of the Board’s ethical integrity and accountability. Dr. Heimbach did all of this unselfishly and without expectation.
Born in Chicago, Illinois, he received his BA and MD at the University of Chicago, where he later returned for a residency in radiology. Drafted into the United States Air Force in 1962, he went on to earn a PhD in Radiobiology at New York University, completed a residency in Aerospace Medicine at Brooks Air Force Base, Texas, and obtained a Master’s in Public Health at the Harvard School of Public Health. Dr. Heimbach became board certified in Aerospace Medicine by the American Board of Preventative Medicine, in 1974.
With his mentor and former residency advisor Dr. Jefferson C. Davis, Dr. Heimbach established the USAF Hyperbaric Medicine Center at Brooks Air Force Base and became its Director of Medical Operations. In this role, he created hyperbaric fellowships for physicians and nurses and authored numerous papers and textbook chapters, all of which contributed to the creation of the hyperbaric medicine specialty. Dr. Heimbach became Director of the USAF Hyperbaric Medicine Center in 1978 and remained in that role until he retired as a Colonel in 1982.
Upon retirement, Dr. Heimbach entered private practice at Southwest Texas Methodist Hospital in San Antonio. His team operated what was, at the time, the only civilian wound care and hyperbaric medicine facility outside a university setting in the South Central United States. He was ably assisted among others by Paul Baker, also late of the USAF, and a long-standing NBDHMT Board Member, including many years as its president. Dr. Heimbach eventually retired in 2000. The last time I spent time with him was a decade or so ago for game of golf along with Paul, a few miles up the interstate from San Antonio.
Dr. Heimbach was one of only two physicians to serve as President of both the Aerospace Medical Association (ASMA) and the Undersea and Hyperbaric Medical Society (UHMS).
The Board offers its condolences to his family, and shares this loss with Dr. Heimbach’s many friends and colleagues. His was a life well lived.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2018
Effective immediately, all CHT, CHT-V and DMT recertification documentation, including wallet cards, will be emailed. The cards can be cut out and laminated in plastic. This paperless transaction is being considered by the BNA Certification Board and will apply to subsequent CHRN recertifications if approved. Please contact Board headquarters if you have any questions related to this new process.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2018
As certification in hyperbaric technology (CHT) is an additional, rather than entry level, qualification, a qualifying pathway is required. The seven options are noted within the Resource Manual on the Board’s web site. For those wishing to become a CHT from outside the medical field the two most accessible options are EMT or LPN.
A question frequently raised relates to maintenance of the qualifying pathway. The majority of pathways are routinely maintained as they frequently represent the primary professional designation and source of primary employment. Respiratory therapists and registered nurses are examples. Where a qualifying pathway has been achieved purely as a basis of CHT eligibility, concurrent employment as an EMT or LPN is uncommon. It is the Board’s present position that maintenance of certification is not required for the CHT recertification.
The Board leaves any decision regarding maintenance of qualifying pathway to the employer and the CHT in question.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2018
All new applications for Board sanctioned training courses go through a detailed review process. It begins with a determination of instructor(s) suitability and assessment of all related course materials, including the student manual. If upon completion of this screening the course in question appears to have merit, and on-site audit is scheduled. One or more auditors will visit to evaluate appropriateness of the facility and delivery of course content. The Board pays related expenses. A course-specific (hyperbaric or diving medicine) audit template is used. These documents serve to ensure that assessment of each course is undertaken in a standardized manner, thereby eliminating for the most part any potential for individual auditor bias.
Upon completion of the audit, a course will be determined to either meet NBDHMT expectations, or fall short. Some courses that the Board sanctions may be required to make changes/additions, but considered relatively insignificant and easily addressed. For courses that fail to meet expectations, a detailed analysis of all areas requiring improvement is provided, with reapplication considered if the changes appear adequate.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2017
December 2017
The Board has received enquiries from those who serve in various hyperbaric and diving administrative leadership positions regarding the awarding of CEU’s for such participation. Examples include membership on NFPA/ASME/PVHO committees, membership on the UHMS Safety Committee, and serving as a UHMS Facility Accreditation Survey Team member.
All of these activities hold importance related to the safety and effectiveness of undersea medicine and hyperbaric oxygen therapy. The Board will, therefore, award continuing education credits, as follows:
For the above noted committees, CHTs, CHRNs and CHT-Vs, will earn one Category A credit for every hour, or part thereof, that such a committee is in session. Attendance at these meetings will need to be verified by each respective chair person, by email to Board headquarters. Credit hours for serving in these capacities will be capped at nine (9) for each respective (CHT/CHT-V/CHRN) recertification period.
For those who undertake a UHMS facility accreditation survey, the Board will award six (6) Category A credits. Confirmation of participation must be provided to the Board by the UHMS Hyperbaric Facility Accreditation Director. Because the survey process is very much template driven, this credit award is a one-time process.
Please let Board headquarters know if you are involved in any other such administrative and oversight functions.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2017
Effective January 1, 2018, CHT/CHRN certification examination decompression table computation questions will be based upon the most recent version of the U.S. Navy Diving Manual. This version became effective December 1, 2016, as Revision 7.
There is no need to be concerned about this if you trained prior to the introduction of Revision 7. The computation process is identical to Revision 6 and only minor changes have been made to various time frames. As the decompression tables included with each test will be from Revision 7 there is no real impact on this updating.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2017
The annual DMT refresher training course has been scheduled for February 7 and 8, in New Orleans. It will be held at the Ernest N. Morial Convention Center, in conjunction with the Association of Diving Contractors International “Underwater Intervention 2018”.
Several of the LSU diving medical officers will again speak, along with two of their Undersea and Hyperbaric Medicine “Fellows”. The second afternoon will also feature an invasive skills practical session. If you have any topics or DMT-related questions you would like to have addressed, please let Board headquarters know as soon as possible.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2017
A Board constituted ad hoc committee has considered the potential and value of Hyperbaric Safety Director certification. After careful review by a committee of hyperbaric leaders it was elected not to proceed with this initiative, at least for the foreseeable future.
What the Board did come up with, however, is a set of expectations for those who provide hyperbaric safety training and seek Board CEU approval. In essence, a set of minimum content requirements have been produced and are included below.
Requirements for issuing continuing education units to Hyperbaric Safety Courses
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2017
In the December 2016 Monthly Briefing, the Board issued a recommendation that no patients, hyperbaric team members, other hospital personal, medical staff members (including cleaning personnel) and visitors be permitted to bring the Samsung Galaxy Note 7 into the hyperbaric facility, including patient change areas.
In January 2017, Samsung said that it had successfully recalled more than 96% of all Note7 devices in the U.S. since this order went into effect, and U.S. wireless providers have pushed out firmware created by Samsung that prevents batteries on the remaining devices from charging.
The Board recommends, therefore, that you contact your hospital’s safety officer to find out if specific policies regarding the Samsung devices have been updated and determine if the previously provided Warning Poster remains necessary.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2017
A heads-up to those who may be contemplating a training opportunity for which NBDHMT approval will be sought.
Traditionally, the Board has granted provisional approval status for all new applications. This status remains in place until a review of post-course critiques for two consecutive offerings has been undertaken. At this point, one of three decisions is made. If the review is favorable the provisional status is removed. If reviews are equivocal, the course director will be provided with guidance to enhance the program’s quality and the provisional tag will remain for two additional offerings and another post-course critique review is undertaken. At this point the course will either be approved without the ‘provisional’ caveat, have one final provisional period, or Board approval retracted.
More recently, all new training courses will be audited by an on-site Board representative. This has become increasingly necessary due to great variance in course quality, the degree of which can only be fully determined by physical presence of a knowledgeable resource.
The Board takes great pride in its certification programs and the quality of its approved educational offerings. On-site auditing is considered a key step to ensure that faculty are knowledgeable of topic and skilled in imparting this knowledge. It also ensures audio-visuals and handouts are complete and appropriate.
The student is the ultimate beneficiary of this due diligence, as are patients of course.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2017
An end of the month Board meeting was held in Naples, Florida. Among items up for discussion was one related to individuals purporting themselves to be CHT’s when in fact they are not.
This misrepresentation is important from several respects. First, it violates the ownership of the CHT Mark, which is held by the NBDHMT. It also suggests that the individual in question has achieved a level of professional training, knowledge, skills and certification that they have not. Finally, it does an injustice to patients who assume that their health care provider is qualified to the degree that they are not.
Because of the Board’s limited resources, it is not able to police the field of hyperbaric medicine. It relies, therefore, on others who may feel that a case of misrepresentation exists. Once alerted, the Board will investigate and take necessary action to preserve the integrity of hyperbaric medicine in general and the CHT program in particular. If you know of any possible misrepresentation, please do not hesitate to contact Board headquarters.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2017
The Board’s annual meeting is scheduled for later this month in Naples, Florida. As is our practice, the meeting will again coincide with the UHMS Annual Scientific Meeting. Agenda items include a proposal to require minimum standards for hyperbaric safety director training courses. While the Board is not presently contemplating a certification program for safety directors we are concerned about varying program quality. In order for the Board to continue awarding educational credits for CHT’s who attend these courses, they will have to meet a set of faculty, course content and topic timelines expectations. It is anticipated that these minimum standards will be available for distribution in the coming month.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2017
Monthly Briefing April 2017 – Note of clarification
A statement in paragraph one of the above referenced ‘Briefing’, included below, stated that an additional requirement exists to accrue a minimum of 12 hours of Category B Credits. How this should have read was; if not all of the necessary 24 recertification credits can be achieved as Category A, then a minimum of 12 Category A would suffice if at least 12 more were represented by Category B. Preferably, of course, all 24 credits should be A.
Example:
Option 1: 24 Category A Credits satisfies renewal requirements
Option 2: 12 Category A Credits & 12 Category B credits likewise satisfies renewal requirements
Hopefully, this will clarify the intent of these two category types.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2017
The CHT is a designation available for allied health professionals engaged in the technical, operational and safety aspects of hyperbaric and hypobaric delivery systems. Intuitively, ongoing skills maintenance and knowledge growth should center around these key practice aspects, and form the basis for awarding CEU credits. CHT recertification requires a minimum of 12 hours of Category A credits, namely those which relate directly to the above skills and knowledge. There is an additional requirement to accrue a minimum of 12 hours of Category B credits, defined as those programs and courses that provide more generalized health care information, if not all of an applicant’s CEU’s qualify as Category A. B credit examples include BLS and ACLS certification/recertification, clinical practice and compliance updates, emerging technologies, and potential new uses.
In the past the board has awarded Category A credits for materials that, while certainly hyperbaric related, did not always address CHT ‘core competency’. This has resulted in CHT’s achieving the necessary recertification credits with little or no technical, operational and safety exposure. Going forward, then, the Board will be more specific as it responds to requests or continuing education credits, in terms of A or B awards. The Board will also require that at least nine (75%) of Category A credits relate directly to technical, operations and safety.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2017
I thought that for this month’s briefing I would share with you some introductory material scheduled to be presented at the upcoming International Congress on Hyperbaric Medicine, in Belgrade. It relates to multiplace inside attendant accidents and injuries, which forms the basis for a Workshop immediately preceding ICHM 2017. The two devastating events noted below occurred in the US and are not as well known, certainly the case in California, as perhaps they should be. I will be discussing operational failures and shortcomings that led to their respective deaths, and what lessons can be taken from them.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2017
This month’s diver medic refresher training course was once again successfully delivered. Some 35 medics representing oilfield, inshore, military, FBI and scientific diving communities attended. Their post-course compliments and praise were uniform and not just because we fed them catfish po-boys and gumbo!
Holding this training in conjunction with the Association of Diving Contractors International “Underwater Intervention” offers several benefits. DMT’s can also register for Underwater Intervention and they get to enjoy Mardi Gras. Most importantly, it is always held in New Orleans so we have ready access to the diving medical experts at LSU/Spirit of Charity Trauma Center. All disciples of the illustrious Dr. Keith Van Meter, they willingly give of their time and expertise each year, and without expectation. The Board is always very grateful for what they do and the diver medics in attendance recognize that they are in the presence of highly trained very experienced and always accommodating subject matter experts.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2017
In case you haven’t noticed, the U.S. Navy Diving Manual recently underwent another revision. This change took effect December 1, 2016, as Revision 7. While there are no material changes to the treatment tables and management algorithms for DCS and CAGE, some changes have occurred to the air decompression tables. For Table 9-7 “No-Decompression Limits and Repetitive Group Designators for No-Decompression Air Dives” several of the No-Stop Limits have been slightly increased (more allowable bottom time). The 25 fsw time has been almost doubled, from 595 to 1,102 minutes.
We will be advising all of the Board’s instructors that the CHT/CHRN examination questions related to air decompression procedures will be switched to Revision 7 effective July 1, 2017. Updated tables will be provided to examinees from that point. Even those who have been trained using Volume 6 should have no difficulties as the methodology to answer the questions in unchanged. Examinees will simply employ whichever set of tables that accompany the tests.
Best wishes for 2017!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2016
December 2016
I am sure that most if not all of you are keenly aware of the Samsung Galaxy Note 7 Smartphone issue. Its potential to self-ignite has resulted in the manufacturer discontinuing production and withdrawing if from the shelves to prevent any further sales. This ban extends to both the original and all replacement Note 7 models. While it is no longer available for purchase and owners have been encouraged to return their units and receive replacements (different models), one has to assume that a large number remain in use. It is important, therefore, that hyperbaric patients are screened accordingly.
The Board recommends that you contact your hospital’s safety officer to find out if specific policies are already in place, and ensure that are adhered to by the hyperbaric medicine service if they do. In the absence of such a policy and to strengthen an existing one, the Board recommends that no patients, hyperbaric team members, other hospital personal, medical staff members (including cleaning personnel) and visitors be permitted to bring the Samsung Galaxy Note 7 into the hyperbaric facility, including patient change areas. It is also recommended that the attached Warning Poster be displayed in a conspicuous place.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2016
The Board has generated a series of Position Statements in recent years. They serve to direct attention to various safety, procedural and compliance issues, the sum of which help ensure that hyperbaric oxygen therapy is conducted in a safe and effective manner. Each Statement is revisited from time to time to be certain that it remains relevant and any citations continue to be up to date. Any edits are identified by a notation in the title as to when they occurred. At the foot of each Statement is the date it was last reviewed if no edits were deemed necessary. You are encouraged to read over these Statements from time to time. In doing so you will note that they last underwent review and editing this month.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2016
A heads-up for you diver medics out there: The annual DMT refresher course has been scheduled for February 22-23. As in the past, it will be in New Orleans in conjunction with Underwater Intervention, held at the Ernest N. Morial Convention Center. We are very grateful to NBDHMT Board Member Dr. Keith Van Meter and his Louisiana State University Undersea and Hyperbaric Medicine Team who will again pick up the lion’s share of the teaching responsibilities. This two day program features diving medicine review and update, extensive clinical skills practical session, and plenty of seafood gumbo and po’ boy sandwiches. For further course details and registration information please visit https://www.nbdhmt.org/forms/DMT_Refresher_Training%202017.pdf.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2016
To be recognized as an approved training course for CHT and CHRN eligibility, providers are required to make a formal application to the Board. In doing so, they must provide documentation that adheres to the necessary standardized course curriculum which includes topic listing and time spent with each topic. The sum of these time frames must be a minimum of 40 hours. Those who wish to be a part of the instructor team must likewise formally apply and be approved. Any subsequent changes within this team that involve four or more hours require re-application. Newly approved courses are screened for quality and compliance by submission of student critiques and the Board reserves the right to audit these courses.
With all of this in place prospective course attendees can feel confident that their educational experience will be a solid foundation to certification testing.
I raise all of this because our Board administrators are asked from time to time to recommend one course over another. They are not able, nor are they permitted, to do so. With adherence to all of the above application and screening requirements there should be little variance between them. If any of these courses become a concern, for one reason or another, the Board would require corrective action where necessary. If any readers of this Briefing are aware of issues related to provision of Board approved training courses I hope that you would let us know.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2016
As noted in previous Briefings, on-line testing is becoming increasingly the norm rather than the exception. Its benefits to examinees include geographic proximity and testing date flexibility. For the Board, this process provides much greater security and control of the examination data base, as well as cost-efficiencies.
There is one issue that has become apparent, one we would like you to share with your colleagues and co-workers who are contemplating hyperbaric or diver medic certification. Because examinees are not locked in to a given testing date/location as is the norm with previously proctored examinations, there is an increasing tendency to change the scheduled on-line testing date. This frequently results in a financial penalty being assessed to the Board. This is not something that we can continue to underwrite. It is important, therefore, that examinees think carefully when committing to a testing date. Going forward, the Board will find it necessary to pass through any rescheduling penalties to the test takers in question.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2016
In follow-up to my June report on some aspects of the BOD meeting, I can share one additional initiative under consideration.
It relates to the ‘Hyperbaric Safety Director’ designation. As you know, one important requirement of the National Fire Protection Association (NFPA 99) is that every facility designate a member of its team to serve in this capacity. Several training opportunities were subsequently introduced to prepare individuals to assume this position. Invariably, the NBDHMT was asked to approve educational credits for those who successfully completed this training. This we did. It is important to appreciate, however, that the NBDHMT does not designate each respective training course as an ‘Approved Hyperbaric Safety Director Course.’ Rather, we award attendance credits, as we would for other educational opportunities.
Great variability is seen to exist between these various safety director courses, in terms of quality of faculty, selection of topics, subject matter completeness and course duration. Accordingly, graduates will have achieved a varied (in-consistent) amount of knowledge.
Accordingly, the NBDHMT has embarked on an initiative to develop a set of minimum training standards. Once they have been completed and introduced, those who offer such training will be asked to ensure compliance in order to continue to qualify their students for ongoing educational credits.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2016
The NBDHMT directors held their annual meeting on June 10, 2016. This meeting provides an opportunity for the Board to sit down around the table in the only scheduled face to face yearly meeting. All other Board communication takes place by email or conference call. Here is a brief review of some reports:
There were 75 testing locations over the past 12 months involving 375 examinees. Since the introduction of online testing in January of this year, 35 of the 55 tests conducted were at online testing centers. The Board expects this method to eventually represent greater than 95% of all subsequent examination opportunities.
As of June 2016 there are 1,543 CHT’s, 611 CHRN’s, 518 DMT’s and 30 CHT-V’s who are both certified and in date.
The third edition (2013) of “Daugherty’s Field Guide for the Diver Medic” has sold 755 copies, (some of which were donated), of the 1,000 copy initial printing. The entire text has recently been revisited by the many chapter authors. Edits have been made and incorporated, as appropriate. A second printing of the third edition will be run as we close in on the outstanding balance.
Several important new initiatives are being contemplated. They will be shared with you via these Monthly Briefing in the coming months.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2016
Online testing is now firmly entrenched within the Board’s certification process. Beginning this month it has been expanded to incorporate veterinary hyperbaric professionals and diver medics. All four certifications are now a part of this process. As we have previously noted, key benefits of online testing are enhanced examination security and flexibility in terms of examinee choice of location and date. This includes overseas locations.
A number of those who had previously registered for group proctor exams have elected to switch to the online option in order to avoid travel costs and additional time away from home/work.
One interesting metric is that there are presently no registrants for the examination to coincide with June’s UHMS Annual Scientific Meeting. This event has historically represented one of the largest number of examinees. All of those who would have chosen this venue now appear to be committing to online testing.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2016
The Board has only recently been made aware of a hyperbaric fire that occurred in August of last year at a veterinary clinic in Holly Hill, north of Atlanta, Georgia. A Sechrist 2500 (their initial model) chamber was being used for animal care. During the treatment of a dog fire erupted within the chamber. As one would predict, the dog did not survive. If there is anything encouraging about the fire it was that the chamber did not fail structurally. This was in all likelihood the result of very little internal material (bedding/clothing commonly associated with human treatments). This incident represents the third reported acrylic hull monoplace chamber fire (all were the 2500 model). One of the three did blow apart, the reason it did was thought to be the unusually large amount of clothing and bedding that had accompanied the patient.
The cause of this particular fire appeared to be a battery operated fan. It was routinely placed inside the chamber to ‘help keep the inside cool’! This clearly violates the basic tenets of chamber fire safety. What was equally alarming, the vet reported that he routinely went into the chamber himself (for what reason we do not know) and with the fan operating.
How the vet came to be in possession of the chamber is not yet clear. It had been used clinically at Crawford Long Hospital in Atlanta and was replaced with a newer model as its 20 year acrylic life cycle had expired. The chamber manufacturer was not aware that is was still in use.
From an NBDHMT perspective, this tragedy certainly serves to validate the value and importance of the CHT-V certification program.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2016
A fire killed four multiplace chamber occupants at Mintohardjo Navy Hospital, in Jakarta, Indonesia on the 14th of this month. Initial reports suggest that an electrical short served as the ignition source. Another report indicated that the chamber’s sprinkler system was activated but did not prove effective. If such a system was activated then these will be the first reported fatalities in a multiplace chamber with an activated water deluge system. An investigation is currently underway so hopefully the full details relating to this tragedy will become available in order that important lessons can be learnt.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2016
We mark the 40th anniversary of the diver medic program this spring. Following a Beta test a year earlier the first DMT course was held in March 1976 at the Commercial Diving Center, in San Pedro, California. Clinicals and lab work was held at USC Medical Center up the road in Los Angeles. After several failed attempts to have the course incorporated into the National Association of EMT’s, the NBDHMT was formed and a certification program for diver medics introduced. The rest, as they say is history. Numerous reports of diver medics successfully intervening in decompression and other diving related emergencies would fill a book. Commercial diving is a safer occupation.
* * * *
On line CHT/CHRN testing is well underway. The Board continues to develop a directory of institutions willing to accommodate examinees and we ask for your assistance. If you are able to locate willing facilities in your region please let Board headquarters know.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2016
We begin this New Year with encouraging news regarding online testing. Within the past several days Beta testing has been successfully completed so we are ready to open up this option to prospective CHT’s and CHRN’s.
Apparently, a significant number of colleges/testing centers do not open their resources to those not enrolled at their colleges. They each have their reasons for this but with a little perseverance testing centers willing to accommodate our examinees can and have been located. You could do a useful service to the Board by calling around within your region to see what opportunities exist for ‘non-enrolled’ test takers. This would allow the Board to compile a nationwide directory, and we would be very grateful for any such assistance.
Our goal is to make on line testing the standard going forward. We will continue to offer ‘hard copy’ opportunities at the UHMS Annual Scientific Meeting and elsewhere if circumstances warrant.
As noted in the previous Briefing, we are working to incorporate the DMT and CHT-V examinations into a online option. Hopefully, this will occur in the coming months.
Best wishes for 2016!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2015
December 2015
As we close out 2015 the Board has some exciting news to share. Beginning in the first quarter of the new year an on-line testing option will become available for those wishing to take the CHT and CHRN certification exams. This process will serve to strengthen testing security and compliance. It will also allow individuals to schedule testing at their convenience. They can use a nearby testing center and avoid having to wait for others to apply before traditional multiple examinee hard copy proctored examinations can be arranged.
We will complete on-line Beta testing within the next 30 days, at which time this process will become widely available. Application forms are being edited to reflect this option. The hard copy proctored option will remain for the foreseeable future but will be gradually transitioned to provision at only the larger hyperbaric meetings. All international examinations will be completely transitioned to on-line testing during 2016.
CHT-V and DMT certification exams will also have an on-line option by the second quarter of 2016.
Many thanks to Board member Richard Barry for prompting this process and thanks to Brandy and Christene at Board headquarters for diligently working on this project.
Very best wishes for the holiday season and the coming year.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2015
I have several updates that relate to certification and recertification requirements that will take effect January 1, 2016. Please share these with your colleagues.
First, those seeking CHT status must now sit the examination within three (3) years of successful completion of an NBDHMT approved introductory hyperbaric training course. Previously this had been an open ended period.
Next, the standard for CHT recertification now requires a minimum of 24 hours of continuing education credits, up from 12. At least 12 of these 24 hours must be Category A (directly related to safety and operational practice of undersea, aviation or hyperbaric medicine). Category B credits relate to topics/subject matter indirectly related to undersea medicine and hyperbaric oxygen therapy. Examples here would include CPR, HIPAA compliance issues, wound care and general medical and safety issues.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2015
A reminder that the deadline for CNA’s and CMA’s to certify as CHT’s is fast approaching. You have until December 31 of this year to take the examination. Effective January 1, 2016 these two allied health categories will be eliminated as CHT qualifying pathways. Also effective January 1, 2016 all current CNA/CMA CHT’s will be required to undergo additional certification or licensure in order to recertify. Examples include EMT, paramedic and LPN.
For the past two years the Board has provided $150.00 stipends to those who obtained these additional certifications. This financial support incentive will also end on December 31, 2015.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2015
Jim Wilson passed away on August 31. Many of you relatively new to diving and hyperbaric medicine will not recognize that name. You ‘old timers’ who were around at the genesis of the NBDHMT and the years that followed likely will.
Jim was one of, if not, the most prominent Canadian pioneers of diving and hyperbaric technology and training. With his colleague and friend Dr. Hal Koch, Jim introduced the first such courses at Toronto General Hospital, some 40 years ago. Jim was of great help as the Board developed its CHT program and served as a foreign representative to the Board for several decades.
Jim’s obituary is attached. Suffice it to say here that he approached all of life’s opportunities and challenges with much enthusiasm and great intent. A perfect first example was the forging of his birth certificate (he was 15 at the time) so that he could fight on behalf of the Canadian armed forces in World War II. He was one of the first Canadian clearance divers, the first Canadian to graduate from the US Navy’s deep diving school and one of the first to dive beneath arctic ice.
The NBDHMT, along with many of today’s hyperbaric and diving practitioners, owes Jim an enormous debt of gratitude. Our condolences are extended to his family. You can read his full obituary here. http://turnerporter.permavita.com/site/JamesHWilson.html

James H. ‘Jim’ Wilson 1927-2015
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2015
A new link is about to be added to the Board’s website. It will allow certified diver medics, hyperbaric technologists, hyperbaric nurses and hyperbaric veterinary technologists to post ads seeking employment. It will also incorporate a section for employers to advertize positions available within their institution or organization. There is no cost to use this service, which can be accessed by completing and submitting a ‘Seeking Employment Form’ from the link.
The Board intends to promote this service to potential employers across the undersea medicine and hyperbaric oxygen therapy disciplines in the coming weeks.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2015
Visitors to the Board’s website in recent weeks will have noticed a sharp new look, particularly when using a mobile device.
The impetus for this change was a threat from Google to punish sites that are not “mobile-friendly” by demotion within their search rankings. The Board’s web master has brought us in compliance with Google and produced a readily good ‘look’ in the process.
…
On another note, follow-up from the Board’s decision to remove CNA’s and CMA’s from the CHT qualifying pathway has been increasingly encouraging. Understandably, there were some who were discouraged and frustrated on first hearing the news. The mood has changed, complaints have turned to compliments. An increasing number are taking this opportunity to advance their professional standing. You may recall that the Board has been providing a $150.00 stipend to help this process. As one of those effected recently wrote “I was not happy when the Board came out with the requirements of additional training, but in order to keep my job I needed my CHT. I am going for my NR EMT and can absolutely see why the Board made the changes and I completely agree that additional training is necessary especially when sitting beside the chambers”.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2015
The Board convened its annual meeting on June 19 in Montreal, Canada. Consistent with previous Board meetings it was held in conjunction with the annual scientific meeting of the Undersea and Hyperbaric Medical Society.
One Agenda item related to the possibility of introducing an on-line certification testing option. The Board had researched this issue some years ago but found it to be prohibitively expensive. On-line testing has evolved considerably since then and more viable products appear to be available. If this is indeed the case any such introduction would serve to complement not replace traditional locally proctored testing. Particularly helpful aspects of any adoption of on-line testing will be the elimination of the waiting period and the need for a minimum of three examinees. More to follow.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2015
We are pleased to report that Joseph D. Snyder, RN, CHT has been elected to the NBDHMT Board of Directors. He brings to the Board almost 30 years of experience in hyperbaric nursing, technology and administrative leadership.
Joe began his career as a corpsman in the U.S. Navy. Upon discharge in 1982 he began his nursing career at Mercy Medical Center, Canton, Ohio, following graduation from Kent State University School of Nursing. In 1987 Joe joined the hospital’s hyperbaric medicine team. He spent 31 years at Mercy before transferring to the hyperbaric medicine service at Akron General Medical Center, also in Ohio, where he remains today. He has been prominent within the Undersea and Hyperbaric Medical Society’s Mid West Chapter, serving as its president from 2003-2005 and again from 2012-2014.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2015
A major milestone in the Board’s credentialing process was passed in the first week of April. Nicole Cairrao, a Rhode Island resident and hyperbaric staff member at Charlton Memorial Hospital, in Fall River, MA, became the 4,000th health care professional to achieve certification in hyperbaric technology. Congratulations Nicole! From its first certification examination in San Diego, in June 1991, the CHT has become the recognized standard of quality and expertise in support of the provision of hyperbaric oxygen therapy.
On a related note, congratulations are also due to Muriel Saliba, a New Hampshire resident and hyperbaric staff member at Elliot Center for Wound Care and Hyperbaric Medicine, at River’s Edge in Manchester, NH. Two weeks ago she became the 1,100th registered nurse to achieve CHRN status. Congratulations are likewise extended to Muriel.
On a final note, for DMT’s out there in need of recertification training, a three day program has been scheduled for July 13-15, 2015. It will be held in New Orleans, LA, and registration details will be available in the coming days.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2015
After several years in development the Board introduced a certification program for veterinary hyperbaric technologists in 2011. This program was prompted by an increasing application of hyperbaric oxygen therapy across a range of animal types, both small and large. Along with this increase in utilization there were concerns regarding adequacy of training and operational safety. Accidents and injuries had occurred and certification was seen as one important step towards enhanced veterinary hyperbaric practice standards.
Since 2011, 16 individuals have become certified as CHT-V’s. At present, this likely represents a small percentage of the total number working in this setting. To emphasize the importance of formalized training and certification one only needs to recall the February 2012 incident in Ocala, Florida, where a horse was being treated. A fire occurred within the chamber, soon to be followed by an explosion and catastrophic chamber failure. The horse died immediately, as did the young lady at the chamber control panel. A second individual was badly injured but survived. Apparently, the explosion was so great that it could be heard three miles away.
Hopefully, there will be increasing interest in CHT-V certification in the coming months and years. Many thanks, again, to Board Member Dr. Dennis Geiser for spearheading this important initiative.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2015
2015 is something of a significant anniversary year.
It was in 1975, exactly 40 years ago, that the first DMT course was conducted. It was jointly provided at Commercial Diving Center (CDC), in San Pedro, California and UCLA Medical Center, a few miles up the road in Los Angeles.
This first course was a Beta test. It involved as students six Oceaneering International diving supervisors, three of whom had been running dives that had resulted in devastating and fatal accidents. Oceaneering was sufficiently concerned about the lack of an on-site diving accident management skill-set to proceed with sponsoring the development of this new program. It lasted three weeks and included a great deal of invasive skills practice within the UCLA animal lab and plenty of hands-on opportunities in their emergency medicine department where it was the ‘Saturday night knife and gun club’ essentially every night. After careful analysis and feedback, the course was finalized and became a fixed offering, regularly hosted by CDC and UCLA. Initially, registration was limited to Oceaneering personnel but was opened up to all diving companies in 1978 as these other companies were offering attractive bonuses to hire away Oceaneering’s diver medic graduates!
Several attempts were made to encourage national organizations representing EMT and other medical first responders to ‘adopt’ the DMT program for certification purposes. All failed. The DMT was too unique a product, one who operated often hundreds of miles from a medical facility and several days from patient transfer (if injured divers were in sat), to embrace.
This prompted formation of the NBDHMT, initially called the National Association of Diver Medic Technicians, in 1985.
To read more of the genesis and evolution of the DMT program go to https://nbdhmt.org/forms/Diver_Medic_Training_and_Certification102010.pdf.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2015
A reminder that the DMT refresher training course is scheduled for February 11/12. As in the past it will be held in conjunction with ADCI meeting at the Underwater Intervention, in New Orleans. The Board is very pleased to report that the diving medicine physician experts at LSU Health Science Center will again take up the lion’s share of the instruction. We have been soliciting which invasive procedures you would like to practice during the skills maintenance session. If you haven’t already done so please pass on your preferences to Board headquarters personnel.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2014
December 2014
As another year draws to a close I would like to express my appreciation to the Board’s administrative team of Christene Gillis and Brandy Whetstone. Ably assisted by Brittany Gamble, they have kept the headquarters office humming like a well-oiled machine. I would also like to thank those who make up the NBDHMT Board of Directors. They consistently give of the time and expertise willingly and without expectation or any compensation. Collectively, they represent the pinnacle of knowledge and expertise across the continuum of undersea and hyperbaric medicine, technology and safety.
Plans for the coming year include another DMT refresher course. Please go to https://nbdhmt.org/continuing-education-center-dmt-recertification-only/ for program content and registration details.
Best wishes for a safe and enjoyable holiday season, and 2015.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2014
The NBDHMT was asked to make a presentation regarding its current certification standards at the Undersea and Hyperbaric Medical Society’s Northeast Chapter Meeting last month.
The timing of this request was good. There is now another technical certification out there so the Board felt this to represent an important opportunity to emphasize what sets us apart. It was also good timing as the Board has just celebrated its 30th anniversary.
During the talk we took the opportunity to include a summary of the genesis of the NBDHMT and the other three certification programs.
The Power point presentation is attached. If you have any questions related to it please email Board headquarters.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2014
The Board is prepared to offer another DMT refresher training opportunity if sufficient interest exists. As in the past, this would be conducted in New Orleans in conjunction with the Association of Diving Contractors International 2015 ‘Underwater Intervention’. The ADCI meeting runs from February 9-12. A 16 hour refresher course would be conducted during two consecutive days within this period. If you are a DMT or DMT instructor and have an interest in attending please contact Board headquarters.
* * * *
The evolution away from CMA and CNA qualifying pathways for CHT continues to go well. Related national training, certification, professional associations and health care purchasers such as Medicare have been uniformly understanding of the need to make this change. Increasingly, CMA/CNA CHT’s see this as a prompt to advance their professional standing in order to maintain CHT status via alternate pathways and thus became more broadly employable within the health care delivery system. As mentioned previously, the Board is providing stipends to those who enroll in nursing and EMT classes to keep their hyperbaric technology certification.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2014
The Board is going to modestly increase the fees it charges for diving and hyperbaric medicine course applications and education credits. It has been almost a decade since the last increase, so this should not be viewed as too painful. While this information applies mainly to the Board’s instructors, it does affect all of you who apply for continuing education/recertification credits. The new rates are already noted on applicable forms (www.nbdhmt.org/nbdhmt_forms.asp) but they will not take effect until January 1, 2015.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2014
A note to follow-up on last month’s Briefing.
The Board has heard from some several CMA/CNA CHT’s expressing discontent. This was certainly to be expected. The Board also heard from an equal number who recognized the rationale behind the change. They indicated that they will seek to advance their professional standing in order to maintain CHT status and ultimately become more ‘marketable’ within the health care delivery system’s medical community with the higher level of training. They were grateful that the Board had elected to provide financial support, by way of an individual stipend of $150.00, to all those affected who agree to enroll in classes to maintain eligibility. There are 190 CHT’s with such eligibility pathway issues and the Board felt that the offer of stipends to all of them was entirely consistent with its stated mission, which is to ‘Ensure that the practice of diving medicine and hyperbaric oxygen therapy is supported by appropriately qualified technologists and nurses, through respective board certification pathways’.
The president of the National Association of CMA’s also contacted the Board as he had been lobbied by one or more of those so affected. He was provided with additional insights. He wrote again to see if grandfathering was a possibility. With an explanation as to why this could not be possible and would make no sense at all he appeared to accept the Board’s.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2014
The NBDHMT has become increasingly concerned that CNA and CMA CHT’s are being placed into clinically responsible positions that exceed their respective scope of practice. The Board considers this to have important patient safety and operational practice implications.
CNA’s are trained to assist with activities of daily living, while CMA’s are trained to assist with clerical work and physician procedures within a medical office setting.
The Board’s earlier decision to include CNA’s and CMA’s as qualifying pathways was thought to represent a means whereby unlicensed personnel could obtain added competency in support of, but not replace, licensed staff. Conferring CHT status was never intended to represent a process whereby CNA’s and CMA’s would, for example, be employed as lead or principal operators of monoplace hyperbaric chambers. Yet this is what has transpired and to an ever increasing degree. This situation does, therefore, warrant corrective action by the Board.
Accordingly, there will be a transition over the next 18 months to an eventual elimination of these two health care categories as eligible for CHT status. The Board understands that this may be somewhat disruptive and concerning to you, however, the Board also knows that it is the right thing to do. The attached document provides a detailed summary of the process whereby this decision was reached. It also suggests an eligibility pathway alternative for CNA’s and CMA’s currently certified as CHT’s in order to maintain their status with the Board.
Designation Qualifying Pathway for CHT (PDF)
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2014
It is not uncommon that diver medics struggle to obtain the necessary hours of DMT instructor-based continuing education required for recertification. Available resources are clearly very limited. In order to improve this situation the Board has introduced a web-based continuing education center. It can be accessed on the Board’s website (www.nbdhmt.org) as a direct left column link, or via the ‘Diver Medics’ link and item #11. At the present time there are seven lectures representing a total of 7.5 hours of credit. To obtain credits diver medics are required to review lectures and complete lecture-specific tests. There is presently no cost for this service. Lecture content and available credits will be increased as suitable material becomes available.
Although the DMT Education Center only went live last week the Board has already received requests from CHT’s for awarding of credits following their viewing of this material. The current topics are very much diver medic related and are not considered to represent suitable Category A ‘hyperbaric’ CEU materials. However, as they do represent an ‘indirect’ knowledge extension they can be used for CHRN/CHT/CHT-Vet Category B recertification credits.
In due course the Board will introduce a similar CEU process for hyperbaric team members.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2014
It is with great pleasure that the NBDHMT welcomes its newest Board member, Bryan Miers. We are delighted with his addition, one that will increase our scope and expertise as we address new education and certification opportunities. Below is his brief biographical sketch.
Captain Bryan Miers is a twenty-two plus veteran of the Henrico County Division of Fire. He also has over 17 years of service as a Nationally Registered Paramedic. In addition to his paramedic, he is a certified Diver Medical Technician (DMT), American Heart certified Advanced Cardiac Life Support (ACLS) and CPR instructor. He is currently the Station Captain of fire station 2. In addition to his suppression responsibilities he is Captain of the Henrico Search Rescue Dive Team. He has been a member of the Dive team for over 10 years. He was placed as team leader in 2011 after his appointment to Captain. Captain Miers has been diving since 1990 and is currently a SDI Instructor. As for public safety diving, he is currently Emergency Response Diver International (ERDI) Instructor and holds multiple certifications from Dive Rescue International. He also holds many specialty instructor certifications including deep diver, dry suit, full face, nitrox, and boat diving. In addition to his scuba diving experience, Captain Miers is a Planning Section Chief (PSC) for a Type 3 Incident Management Team (IMT) team, which oversees emergency response to large incidents throughout the Central Virginia Area. He has also received specialized training in swift water rescue from Rescue 3 and Marine Patrol functions from the US Coast Guard. Captain Miers has worked with the Virginia Port Authority and numerous dive teams throughout the state of Virginia to increase the safety of Public Safety Divers. He was instrumental in the development of the Richmond Metro ‘Dive Accident Management Manual’, a unique and valuable document that effectively guides both the medical first responder and the areas public safety dive team members when faced with a diving accident or injury. Captain Miers will bring his knowledge and skills to the development, introduction and oversight of the Board are new diving medicine certification courses for shore-base medical first responders.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2014
As we close in on the 25th anniversary of the certified hyperbaric technologist program it was thought useful to provide a brief summary of its beginnings, evolution and present status.
Deliberations by the National Association of Diver Medic Technicians represented the genesis for this category of allied health professional. Constituted in 1985, the NADMT served as the oversight organization for the medically and geographically remote diver medic. Within its leadership were several representing the operational and clinical practice of hospital-based hyperbaric medicine and all too aware of a lack of formalized training standards and certification for those who operated hyperbaric delivery systems. Arguably, hyperbaric medicine represented the last therapeutic service without such standards.
Over an 18 month period working groups were tasked with the development of eligibility criteria, training modules, instructor approval standards, an examination question bank, a study guide and additional program resource materials.
Once these components had been assembled the CHT program was launched. Initial certification testing took place in San Diego, California, in conjunction with the Undersea and Hyperbaric Medical Society’s 1991 Annual Scientific Meeting. At this time the NADMT became the National Board of Diving & Hyperbaric Medical Technology, a non-profit certification organization. First headquartered in New Orleans, LA, the Board’s administrative home was relocated to Columbia, SC in 2009.
In 1995 the NBDHMT had assumed responsibility for the hyperbaric nursing certification testing process, on behalf of the Baromedical Nurses Association and its Certification Board. A certification program in veterinary hyperbaric technology followed in 2011.
Consistent with other medical technology certification standards, CHT’s are required to maintain competency and commit to ongoing education. They do so through recertification requirements based upon confirmation of skills maintenance and accumulation of hyperbaric-specific education credits. To facilitate ongoing professional development, the NBDHMT accredits numerous online enduring material programs, and likewise credits various meetings and conferences.
The NBDHMT assumes a leadership stance on all things hyperbaric safety and related operational practice, which includes ongoing generation of Position Statements. (www.nbdhmt.org)
Practicing CHT’s are encouraged by the fact that their certification Board is comprised largely of their hyperbaric technology peers, peers who represent an enormous amount of experience and expertise. They are joined on the Board by others widely acknowledged as undersea and hyperbaric medicine subject matter experts. Board members offer their time and expertise freely and without expectation. They receive nothing in return but the satisfaction that hyperbaric treatment facilities and their patients are that much better off because of the existence of an exacting certification in hyperbaric technology.
Over the past 23 years 3,797 individuals have achieved hyperbaric certification status, 126 (5%) doing so ‘With Distinction’. Unfortunately first time failure rates have steadily increased over the past decade. From a rate as low as 8-10% in the 1990’s, they have reached 25% in recent years. Retake failure rates are likewise significant for a steady increase. Analyses of respective qualifying pathways indicate that rates are highest among certified nursing aides and certified medical assistant categories, where they approach 60%. This is in stark contrast to registered nurses who choose to take the CHT examination, where pass rates consistently exceed 98%. Because of this growing problem with CNA’s and CMA’s, the Board is currently undertaking a reassessment of its earlier decision to open up certification testing for these nursing support categories. This is high on the Board’s agenda as an increasing number of hospitals are using them in an all too frequent unsupervised hyperbaric chamber operator role. All of those who initially fail are advised of their weakness, encouraged to commit further study and scheduled for retesting upon request and following a minimum of six months from their first attempt.
Those who fail a second time must attend a second NBDHMT-approved hyperbaric training course before becoming eligible to sit the CHT examination for a third and final time.
In conclusion, the practice of hyperbaric medicine is supported by a long-standing and reputable hyperbaric technology certification process. This not-for-profit program’s leadership is comprised largely of CHT peers and representing an enormous amount of experience across the continuum of undersea medicine and hyperbaric oxygen therapy. The essential ‘center of gravity’ of the Board’s mission is to ensure that the practice of hyperbaric medicine has ready access to chamber support personnel who have achieved certification and commit to ongoing skills maintenance and knowledge expansion.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2014
An eligibility update for those wishing to take the Certified Hyperbaric Registered Nurse (CHRN) examination has been introduced. Effective January 1 of this year, applicants must apply within five years of completing their NBDHMT approved hyperbaric medicine training course. Dispensation is available to those who exceed this five year rule if proof of at least 60 hours of hyperbaric medicine (Category A) educational credits can be provided. Nursing School transcripts would not be considered acceptable in this regard.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2014
For the first time one of Medicare’s national contractors has incorporated into its Local Coverage Determination a requirement that staff members operating chambers be trained and certified in hyperbaric medicine. Each Medicare Contractor produces an essential interpretation, or clarification, of national CMS/Medicare reimbursement policy. This is contained within each respective Contractor’s LCD. All of those health care facilities and professionals practicing within a Contractors region of jurisdiction are required to maintain compliance with the dictates of their governing LCD.
Novitas Solutions is the Contractor in question. Their new LCD is presently in draft form. Open hearings have been completed, with the NBDHMT represented and presenting at one venue. The Board expressed its approval and encouragement of the training and certification standards and made several content and language recommendations. A final LCD is expected in March.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2014
The Board is pleased to advise that a new certification program is currently under development. It involves training in diving medicine and is directed at the shore-based first responder.
This program is considered necessary as there is presently no other formalized certificate training in this unique area of medical first responder practice. Not infrequently, EMT/paramedic units are called to inland bodies of water and coastal zones to evaluate and transport injured divers. Commonly, these first responders are not familiar with the etiologies resulting in decompression illness or other diving-related injuries. Consequently, there may be some delay as until clinical picture is better clarified, appropriate immediate management instituted and destination protocols determined.
In recent years a number of these first responders and public safety personnel have undergone Board approved diver medic (DMT) training. While the Board certainly appreciates this degree of interest, the Board also recognizes that the current DMT program offers little in relevance to the practice patterns expected of shore-based personnel. The DMT program’s genesis and current basis is the training of medically and geographically remote commercial/professional dive team members, and those who directly support these teams. The DMT is trained to practice in and around the diving chamber as the eyes, ears and hands of a distant medical control physician. This is a far cry from shore-based medical first responders, whose remit is to function within the immediate pre-hospital setting; where hand-off to a physician is usually minutes rather than hours away. Injured professional divers may find themselves many hundreds of miles from a hospital, with several days of decompression required before they can even begin their medical evacuation journey.
Not surprisingly, shore-based first responders who have undergone the current diver medic training program have had difficulty with its unique concepts, operational settings and practice expectations of the remote duty DMT.
The Board is in the process of developing a suitable core curriculum, training course outline, related time frames and an instructor approval process. It is hoped that this process will be completed by May 1 of this year. Please stay tuned for additional updates.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2013
December 2013
2013 has been another busy year for the Board. A record 66 locations were scheduled for CHT, CHRN and CHT-Vet certification testing. The second DMT refresher training course was held in New Orleans, and included attendance by Board-approved DMT instructors, who were preparing to teach consistent with the Board’s DMT certification examination. Effective 2014, DMT certification will require standardized testing, as per CHT/CHRN/CHT-Vet testing, and no longer based upon each instructor’s individualized post-course test.
Since its availability in April of this year, some 250 copies of ‘Daugherty’s Field Guide for the Diver Medic’ have been purchased. This third edition was completely revamped, updated and expanded, resulting in a doubling of its previous page count.
Best wishes from Board headquarters for the holiday season and the coming year.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2013
An update was recently made to the CHT Resource Manual. It related to the process whereby those who have failed to recertify can regain CHT status. The change applies to those whose certification has lapsed for more than two years. In order to recertify, it is now necessary to begin the application process from scratch. This means that applicants must have a current qualifying pathway and should have completed a Board approved hyperbaric training course within two years of their re-application date.
Questions occasionally arise as to the definition of categories of continuing education credits. Two such categories exist. One is termed Category A. To acquire Category A credits one must be exposed to topics/subject matter that is directly related to undersea medicine or hyperbaric oxygen therapy. Examples include chamber fire safety, patient chamber complications, hyperbaric operational issues and emergency procedures, and updates on indications for HBO therapy. Category B credits relate to topics/subject matter indirectly related to undersea medicine and hyperbaric oxygen therapy. Examples here would include CPR, HIPAA compliance issues and wound management updates.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2013
There is occasional confusion regarding the training course approval processes of the Undersea and Hyperbaric Medical Society and the NBDHMT. Each organization is a separate entity and directs their course approvals to very different groups. The UHMS approves hyperbaric medicine and other courses for physicians, through its relationship with the American College of Continuing Medical Education. This course approval process represents the pathway for physicians to become eligible for hospital credentialing in undersea and hyperbaric medicine.
The National Board, on the other hand, approves courses that represent the pathway for certification in hyperbaric technology (CHT) and hyperbaric nursing (CHRN). These two organizational approvals are independent and exclusive of one another. A nurse or technician would not be eligible to sit their respective hyperbaric certification exam by attending a UHMS approved course, unless that course was also approved by the National Board. Many courses are approved by both organizations, some are not.
Likewise, a physician would not be eligible for education credits and probably not be eligible for hospital credentialing if he/she attended a National Board approved course that was not concurrently approved by the UHMS.
* * * *
A reminder to diver medics that our third annual DMT refresher training course is scheduled for February 10-11, 2014, in New Orleans. Registration details are available at https://www.nbdhmt.org/forms/DMT_Refresher_Training_2014_Application.pdf. The Board will provide each registrant with a copy of the 2013 Daugherty’s Field Guide for the Diver Medic as a function of their registration fee.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2013
Long silent on the issue of off-label HBO therapy, the Federal Drug Administration has finally spoken up. In the first of two recent publications consumers are cautioned as to the likelihood of being misled by promoters of off-label hyperbaric ‘treatments’. This ‘Consumer Update’ lists some 23 conditions being touted as likely to benefit, with the FDA noting that all lack supportive clinical evidence.
As medical science has invariably failed to find therapeutic answers for these conditions it is perhaps not too surprising that many desperate patients and their equally desperate families will grasp at any proverbial straw. Sadly, there are always those who see these patients as an easy source of revenue. This publication makes reference to a growing number of disgruntled patients and frustrated health care professionals who have formally complained to the FDA.
In a second off-label related issue, the FDA has issued warning letters to Healing Dives, Inc. (Woodland Hills, CA), Hyperbaric Options (Troy, Michigan), Oxyhealth, LLC (Santa Fe Springs, CA) and Pressure Tech, Inc. (Freeport, NY). These four companies manufacture/market products to those who have been led to believe, or would like to believe, that breathing 4 psig air inside an inflatable chamber is somehow therapeutic. The FDA accuses these companies of adulteration and/or misbranding of their respective 510 (k) status.
The two links below will allow you to read these publications in full.
http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm364687.htm
http://www.fda.gov/ICECI/EnforcementActions/WarningLetters/2013/ucm20035841.htm?Page=1
Hopefully, the FDA will continue to use its authority to enforce standards that serve protect consumers and guide the appropriate application of HBO therapy.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2013
One other issue addressed during the June BOD meeting was the high CHT examination failure rates amongst CNA’s and CMA’s. These rates frequently exceed 50% and it is common for those who do not pass to fail subsequent attempts. Board members considered whether there were problems with preparation to take the examination, aptitude shortcomings, inadequate preceptorship, poor internship oversight, some other issue(s), or a combination of these factors. As essentially all other qualifying pathways enjoy quite a high overall examination success rate, it was felt by many on the Board that the CNA and CMA level of medical training might just be inadequate for assumption of a CHT role. It was pointed out that there is probably nowhere else in hospital and hospital-affiliated settings where these two categories of allied health employees are able to practice at such an advanced and somewhat independent level as that of a hyperbaric chamber, with related and someone independent patient care.
In fact, the CMS/Medicare web site specifically states that the CNA is not a professional, per se, and does not have a scope of practice. CNA’s are certified not licensed and are employed to assist nurses. It is the nurse’s license that the CNA works under. CNA’s are to perform only those tasks that state laws and regulations delegate to them. These tasks are usually limited to personal hygiene and activities of daily living for patients.
The result of these discussions is that it was elected to maintain CNA’s and CMA’s as qualifying pathways for the time being and to continue to closely monitor respective certification examination results. However, it was decided that effective immediately these pathways will now require at least 12 months of active employment as a CNA or CMA before becoming eligible to sit for the CHT examination. In the meantime a task force will be constituted by the Board to evaluate the greater national regulatory and compliance issues of these allied health designations with respect to the practice of HBO therapy.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2013
We have found it necessary to edit the April 2010 Position Statement, one entitled ‘Physician Attendance and Supervision of Hyperbaric Oxygen Therapy’. This statement refers to the importance of physician presence in order to affect the safe and effective application of HBO therapy. The Board considered that the language was self-evident, namely, that physician ‘presence’, is required, which we considered as clearly implied in the title ‘Attendance’. However, the language of the statement has been argued in one instance as not to actually require that a physician is present and readily available. Rather, our Statement was considered to imply that being ‘readily available’ by phone would meet intent. Of course, this is far from our intent and completely inconsistent with safe practice standards. So, and in order to avoid any possible future misinterpretation, the statement has been revised, effective July 2013. It is provided below and has already been posted on the Board’s Home Page.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
* * * * *
Physician Attendance and Supervision of Hyperbaric Oxygen Therapy: (2010-01) April 2010 (Rev. July 2013)
It is the position of the National Board of Diving & Hyperbaric Medical Technology that provision of hyperbaric oxygen therapy must be directly supervised by a physician (or nurse practitioner/physician assistant where permitted by prevailing credentialing and regulatory standards) who is formally (UHMS or other authoritative body) trained in hyperbaric medicine, involving a face to face classroom vs. online setting. Such supervision should extend to:
- Assessment of suitability for HBO therapy
- Determination of risk-benefit profile
- Interpretation of any related diagnostic testing
- Generation of a therapeutic dosing profile
- Evaluation of subsequent clinical course, and
- Management of any related side effects and complications
Further, the hyperbaric physician must be on the premises and immediately available to the chamber facility at all times that the chamber(s) is occupied. Immediately available would meet the intent of this Position Statement if the physician could arrive at the chamber facility within five minutes of being summoned and in doing so, would not place in jeopardy any other patient presently under their care.
It is the duty of hyperbaric nursing and technical personnel to safely implement ordered therapy and closely monitor patients during their treatments. Should a patient voice complaints or manifest signs suggesting an unanticipated change in status, considered to be hyperbaric related or otherwise, the hyperbaric physician should be immediately notified. Importantly, hyperbaric nursing and technical personnel do not assume any of the physician responsibilities noted above and cannot initiate hyperbaric treatment without patient-specific hyperbaric physician signed medical orders.
June 2013
The Board of Directors held their annual meeting in Orlando earlier this month. The agenda was packed with reports, items and issues in need of discussion and reconciliation. Several of them are listed as bullet points, below:
- A record 62 testing sites were scheduled for CHT/CHRN/CHT-V testing over the past 12 months, involving 205 examinees.
- In the first month of its availability 107 DMT Field Guides were purchased.
- The financial health of the Board remains strong and will allow continued support of mission-related projects identified by, or requested of, the Board. In the past 12 months the Board has invested some $50,000.00 in such projects.
- Given the consistently high CHT examination failure rates associated with licensed practical nurses and certified nursing aides, the Board discussed whether these eligibility pathways should be revoked. It was eventually decided to allow their continued access to CHT testing. However, they are required to have first accrued a minimum of one year’s employment experience in the traditional role of an LPN or CNA before employment in hyperbaric medicine, related training and the 480 hour preceptorship period. The Board thought it reasonable to require this one year of experience standard to all CHT eligibility pathways.
- The Board will again sponsor a DMT instructor refresher training opportunity. Earlier this year 11 instructors were finally supported to attend such an update. They joined a number of DMT’s as they underwent update training, in New Orleans. The Board will offer these same opportunities in conjunction with the January 2014 ADCI program, again in New Orleans.
Additional Board meeting update material will be provided in next month’s briefing.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2013
The NBDHMT is very pleased to introduce you to a new member of its Board of Directors. Dr. Sean Hardy was elected several weeks ago. Sean is board certified in emergency, undersea and hyperbaric medicine. He was first a paramedic then attended medical school at the University of Texas Southwestern Medical School at Dallas. He interned at Louisiana State University/Charity Hospital, in New Orleans, and remained there to complete residency training in emergency medicine. This was followed by undersea and hyperbaric medicine fellowship training, also at LSU.
Sean has completed both the National Oceanic and Atmospheric Administration’s diving medical office training course and the Undersea and Hyperbaric Medical Society’s diving medical examiner course. He practices with long-standing Board member Dr. Keith Van Meter’s team, in New Orleans. His related interests are evident from additional training and certifications, which include FEMA incident command systems training and advanced SWAT team-Department of Homeland Security training and certification.
Sean lectured during the January 2013 NBDHMT sponsored DMT instructor refresher and DMT update training course, in New Orleans. This is where he caught our eye. He has since updated, very effectively, the invasive skills chapter in the new (Third Edition) of Daugherty’s DMT Field Guide (available this week!).
The Board is delighted to have on board someone of the caliber of Dr. Sean Hardy. He is a knowledgeable, personable and enthusiastic physician, a great advocate of the diver medic training and certification program, and an experienced DMT medical control physician.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2013
It has been a particularly busy time at the Board headquarters as the new edition of the DMT field guide underwent final editing. We were beginning to think that there is no such thing as a ‘final’ where editing is concerned! The text is now at the printers and we expect to begin shipping copies before the end of this month.
Many of you who are working in the hyperbaric medicine setting may be aware of the sudden controversy regarding the use of HBO therapy for diabetic foot ulcers. A recent paper in the journal “Diabetes Care” (Margolis DJ, et al. February 19, 2013) reported HBO’s failure to heal wounds and prevent amputations, following a retrospective review of over 6,000 cases. This data is in marked contrast to results from higher quality data (retrospective studies being less regarded than randomized, controlled trails). One seemingly apparent reason for this contrast in outcomes is a failure to incorporate transcutaneous oxygen (TCOM) testing during the evaluation and case management of these patients. The NBDHMT has long recognized the importance of this screening tool, having mandated its training as a part of the eligibility criteria for CHT status over a decade ago. Encouragingly, two equally recent papers have found HBO to be clinically valuable in this same condition. One was a randomized and controlled trial (high evidence level) where TCOM screening was employed and where HBO patients clearly did better than those allocated to “controls” (Ma L, et al. Ostomy Wound Management, March 2013). The second paper is an analysis of all previously published randomized and controlled trails. The authors conclude that “…HBO improved rate of healing and reduced risk of major amputations…in selected patients…” (Liu R, et al. Mayo Clinic Proceedings February 2013). It does appear that TCOM screening should be incorporated if diabetic foot ulcer patients are to be best managed.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2013
The third edition of the DMT field guide will go to the printers later this month. Twenty subject matter experts have reviewed, edited, updated and in some cases completely re-written the chapters that made up the second edition (vintage 1992). Others have produced entirely new chapters and appendixes. All of them have freely given of their time and expertise without expectation, although they will get a free copy! We expect that the guide will be available by late April so the Board is now accepting orders. See the link below for pricing and ordering information.
https://nbdhmt.org/forms/Field_Guide_Order_Form.pdf
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2013
Last month’s combined DMT instructor updating/practicing DMT refresher training and skills updating course was a great success. All of the speakers were excellent. They brought the highest possible knowledge and practical experience to an eager audience.
The DMT instructors were sponsored by the NBDHMT in order to prepare them for teaching students based upon the national DMT certification examination that goes into effect in the coming months. Instructors were updated as to current standards for evaluation and immediate management of diving accidents and injuries. Each lecture incorporated sample questions from the certification exam. The DMT’s were likewise updated and enjoyed the opportunity to practice various invasive skills, kindly coordinated by Safety Management Systems.
Elsewhere, the editing and revising of the third edition of the DMT field guide gains momentum. We expect to have it completed by the middle of this month. Layout and editing should be finalized by late March. This will put us on track for its publication and availability in May. You can preview the front cover and the original photograph at https://nbdhmt.org/dmt_cover.asp.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2013
The CHT Code of Conduct is a set of principals, values, standards and responsibilities required of all hyperbaric technologists who are certified by the National Board of Diving & Hyperbaric Medical Technology. Among other things, the Code of Conduct serves to ensure that patients are treated safely and operational practices are in compliance with prevailing codes and standards.
In recent months, the Board has found it necessary to discipline two CHT’s, both of whom had violated several aspects of their Code of Conduct. In administering respective sanctions the Board recognized that in each instance the CHT’s management had, in effect, placed their employee in direct conflict with the Code of Conduct. They had done so by permitting the hyperbaric facility to operate in the presence of serious compliance and safety violations. Given that employees have little to minimal influence over a facility’s operational and safety policies, the Board considered it necessary to inform the employer of some of the circumstances that led to disciplinary procedures being implemented against their employee. Facility management was urged to rectify such violations in order to improve patient safety and not place other staff members in violation of their Code of Conduct.
The Board takes its safety and compliance leadership responsibility very seriously. The introduction of the CHT Code of Conduct and expectations of compliance is one tangible example.
Happy New Year!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2012
December 2012
Season’s greetings from Board Headquarters! We hope that you and your families will have a safe and enjoyable holiday season.
This past year has been a particularly busy one. A record 49 testing sites were scheduled and 2013 is shaping up to be equally busy. This has resulted in a particularly large number of certifications to process but our administrative team is up to the task. Since the Board’s relocation to South Carolina we have strived to fully automate all related activities. From the 40 plus filing cabinets previously, we have just two now. The Board is operating on a foundation of 2012 hardware and software standards and capabilities. Hopefully, you have sensed some of this with our particularly prompt turn-arounds for certification and recertification applications. The ability to electronically confirm certification has also been well received by potential employers and others.
One final reminder regarding the upcoming DMT refresher course, January 16/17, in New Orleans. Registration information and a course outline are available at https://nbdhmt.org/forms/DMT_Refresher_Training_2013.pdf.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2012
A reminder that the second annual DMT refresher training course is coming up in January. As with the previous course, it will be held in New Orleans in conjunction with the Association of Diving Contractors International ‘Underwater Intervention’ conference. The location is the Morial Convention Center and the dates are January 16-17. Updates on the evaluation and management of the injured diver will be followed by a series of clinical skills refresher sessions using a variety of teaching manikins. For additional details and registration information please go to https://nbdhmt.org/forms/DMT_Refresher_Training_2013.pdf.
* * * * *
The editing of ‘Daugherty’s Field Guide for the Diver Medic’ is about to get underway. This will represent the first revision and upgrading of this very popular text in over 20 years. New sections will be added and the evaluation and management aspects will be brought completely up to date. This process is expected to take several months, as all of those involved have ‘day jobs’, so are volunteering their respective personal time. As in the past, the Guide will be printed on waterproof and tear proof synthetic paper. I will keep you updated via subsequent Monthly Briefings as to an anticipated publishing date. If any of you who have a current version of the Guide would like to see information included that is not presently available then email the Board (www.nbdhmt.org) with your suggestions. We welcome them!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2012
The Board has recently clarified and defined its CHT recertification process. This was prompted by one or two lapsed CHT’s seeking to get their certification back, in one case involving over a decade of inactive status. Listed below is the recertification process and options available to those who fail to recertify within the initial required time frame.
Certification in hyperbaric technology is awarded for a two year period. Recertification applications should be received at Board headquarters no later than the final date noted on the CHT wallet card. If you have lost it then go to www.nbdhmt.org and the ‘Confirm Certification’ link. Enter your name in to the Confirm CHT Certification and this will display your CHT expiration date. In those who fail to recertify by this date a one year grace period is extended, and a $100.00 late application penalty assessed. Upon expiration of the one year grace period, one final option remains for those laggards still wishing to recertify. This option only applies to those who have maintained active certification or licensure in a qualifying pathway. In this instance, the applicant is required to retake the CHT certification examination. Upon successful testing these applicants would be reinstalled as CHT’s. All others, including those who did not maintain active certification or licensure in a qualifying pathway following expiration of the grace period, must begin the process of regaining CHT status via an entirely new application.
While the Board will make an effort to alert CHT’s that their recertification date is approaching, the final responsibility is that of each individual. Military personnel deployed in the Middle East are contacting Board headquarters to ensure that their CHT status doesn’t lapse, for goodness sake. If they can do that with everything else that they have to deal with in their lives, it is difficult to be sympathetic with those who enjoy the daily comfort and safety of their own workplace and home, largely on the strength of those who are deployed overseas.
A CHT is one who continues to maintain required training and educational standards and continues to maintain a minimum level of hyperbaric-specific employment. The sum of this is that their skill set is likely maintained, if not elevated, and patients can expect (as they should and as they deserve) to be treated in a safe and effective manner. Failing to maintain CHT status beyond the scope of the above referenced recertification periods and expecting to have it immediately returned after a period of several to many years brings into question a hyperbaric technologist’s current competency level and longer term commitment to this discipline.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
September 2012
The Board is delighted to announce that it has acquired the rights to Dr. Gordon Daugherty’s ‘Field Guide for the Diver Medic’. This vital resource was first published in the 1980’s and revised in 1992. It became an essential part of the ‘tool kit’ for a great many DMT’s, selling more than 6,000 copies in over 30 countries during the ensuing 25 years.
Author Gordon Daugherty taught DMT training courses on behalf of Houston, Texas-based ‘The Ocean Corporation’ at the time that he wrote the guide. He also served on the Board of the NBDHMT during this same period. Dr. Daugherty has long since retired and resides in Austin, Texas. He was delighted to learn that his work will live on and readily agreed to sell his ownership rights.
As the material is now 20 years old it is in need of a great deal of revision and updating. Plans are underway to have this accomplished and we anticipate that the new edition will be printed early in the New Year.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2012
This month’s Briefing will continue with updates on key aspects of the June Board of Directors annual meeting. In last month’s Briefing two important mission-related initiatives were described.
It was felt necessary to generate a new Position Statement, the first for 2012. This one urged that all those who work within clinical hyperbaric chambers, and others who might be called upon to do so, be medically cleared as fit for employment in this unique environmental setting. While many hyperbaric medicine programs already incorporate such screening not every program does. The Board felt it important to take this position as a means of enhancing the safety and well-being of those above mentioned personnel. (See Position Statement 2012-01; July 2012).
One other initiative was to formalize the curriculum and improve availability of training for those who wish to certify as hyperbaric veterinary technologists. As in the past, Board Member Dr. Dennis Geiser and his committee members have been working to complete various veterinary-related certification components. In the meantime it is considered necessary to provide training opportunities in conjunction with Board approved human hyperbaric courses. The plan is to have the first three days scheduled as a common track. The next two days will be split into human and animal tracks. Two veterinary specialists will travel to respective locations in order to provide the animal course content. The Board is currently making the necessary arrangements for this combined course to be offered twice annually until the full animal-only course achieves Board approval.
On a final note I want to advise you that Paul Baker has resigned his position on the Board, effective July of this year. Many of you will be familiar with Paul’s many accomplishments over almost five decades of military and civilian hyperbaric operations. For 15 years Paul was at the helm of the NBDHMT. That position was passed over to me in 2009 while Paul continued to serve your interests as the Board’s at-large member. Very many thanks, Paul, for your long-standing and unselfish commitment to NBDHMT mission.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2012
This year’s Board of Directors meeting was lengthy (some four hours) and productive. The agenda was packed with important items which collectively served to consolidate existing Board certification processes and both advance and broaden our training and safety responsibilities. Over the next several ‘Briefings’ I will provide detailed updates on some of the more significant decisions that were agreed upon, and will start out with two this month.
The Board’s financial position is healthy enough that additional resources are to be directed at further improving mission-related educational activities. Accordingly, we are going to develop and introduce a series of on-line lecture presentations that will also serve as NBDHMT Category ‘A’ educational credits. They will be accessible through the Board’s website and be free of charge. Subsequent to this initiative, those who seek to recertify will be required to submit evidence (by way of printable certificates) of completion of a select number of these presentations, which will be continually expanded upon. This process is designed to update diver and hyperbaric medicine personnel to key operational, safety, compliance and technical advances. It will also improve access to the necessary Category A CEU’s required for recertification, something that has proven problematic for a number of you over the years.
A second related initiative is a plan to convene a conference for all of the Board’s approved DMT instructors. The objective here is to bring instructors up to date with regard to the duties and responsibilities of the DMT, as they relate to the evaluation of the injured diver, communication with the diving medical officer and optimizing medical management, all from a 2012 perspective. This conference will also serve to better prepare instructors to address and upgrade course content in order to become complaint with the standardized DMT certification examination. The Board intends to underwrite the conference registration fee, hotel accommodations, and offset a significant portion, if not all, of related air travel costs, so that instructors will not be out of pocket. It is anticipated that this conference will also be open to DMT’s for refresher training, on a first come-first served basis.
Dick Clarke, CHT, President
National Board of Diving and Hyperbaric Medical Technology
June 2012
I’m compelled to share with you a recent and disturbing event. A hyperbaric team member in Florida contacted a national resource for guidance. His question related to the issue of air breaks, and I have to assume that he was referring to the monoplace hyperbaric delivery system. He related that two physicians in his center would not allow this simple, inexpensive and valuable safety technology to be incorporated unless ‘it was the law’. Absolutely fascinating! Patients would not be afforded this largely standardized approach to hyperbaric operations unless the respective hands of these physicians were forced by some form of ‘legal’ precedent (as if law-makers dealt with such things in the first place).
As informed readers you will no doubt grasp the absurdity of this situation. Why on earth would these physicians not consider this well established safety tool, one costing a mere several hundred dollars? Surely, they were not going to have to pay to have it installed. The caller was eventually referred to our Position Statement on air breaks (August 2009). This particular Statement points out that every hyperbaric chamber should be equipped with an air breathing capability. The caller was also provided with pertinent literature citations. Introducing air breaks should surely not be something the hyperbaric physician is forced to do, something based upon rules and regulations. It should be something that they should see fit to do in the interests of enhanced patient safety. Hopefully, the hyperbaric safety director was able to prevail.
Dick Clarke, CHT, President
National Board of Diving and Hyperbaric Medical Technology
May 2012
The May 1, 2009 Florida monoplace hyperbaric chamber fire and double fatality has resulted in criminal charges being filed. The hyperbaric medical director and the hyperbaric safety director have been arrested on charges of aggravated manslaughter and manslaughter. A review of the Probable Cause Affidavit reveals an astounding and unbelievable litany of safety and practice standard failures and violations. It was almost a primer in how not to practice.
Some examples include the presence of only one hyperbaric technician, one trainee technician and no nurse in the presence of 12 monoplace chambers; the absence of the technician at the time of the fire; the failure of the trainee to comprehend how to emergently decompress the chamber, resulting in a delay that may well have contributed to non-survivable burn injuries; the chamber in question having long been operationally deficient and should have previously been removed from service; a faked inspection processes; failure to ground the chamber’s occupants, and on and on.
The threat of a catastrophic hyperbaric chamber fire is ever present, as this tragedy attests. It is mitigated to the greatest extent possible by the incorporation of a comprehensive safety plan and an inherent safety culture throughout the entire hyperbaric team. Chambers and related equipment need to be designed, constructed and certified in accordance with prevailing codes and standards. Once operational, they should likewise be maintained and serviced consistent with prevailing codes, standards and authoritative guidelines. Personnel must be appropriately trained and apply their training in every instance to optimize the safe operation of the hyperbaric delivery system. This includes careful record-keeping and the immediate withdrawal of chambers or ancillary equipment from service if problems or concerns are identified. Such equipment should only be returned to use following approval by relevant authorities.
Consistent with the position of the National Board of Diving and Hyperbaric Medical Technology, clinical hyperbaric facilities should undergo a UHMS accreditation survey at the earliest possible opportunity. It is this form of authoritative external review that is best able to confirm, or otherwise, that facilities are operating within expected levels of clinical practice and operational safety.
One cannot emphasize enough the importance of a culture of safety within the hyperbaric medicine environment. That the vast majority of hyperbaric treatments are provided in an uneventful manner can and has lead to complacency. This problem may compound itself if events lead to a lowering of operational practice standards via the introduction of lesser trained individuals, understaffing for economic gain, and failure of an ongoing commitment to continuing education and skills maintenance. The NBDHMT’s mission is, in large part, to provide every opportunity to facilitate high quality, efficacious and safe hyperbaric operations.
Dick Clarke, CHT, President
National Board of Diving and Hyperbaric Medical Technology
April 2012
The annual NBDHMT Board of Directors meeting is scheduled for June 21. As in the past, it will coincide with the scientific meeting of the Undersea and Hyperbaric Medical Society. This year’s venue is Phoenix, Arizona. Continuing another tradition, we will host a ‘Breakfast with the Board’ the following morning, Friday June 22. This represents a great opportunity for those of you planning to attend the UHMS meeting to say hello to the directors and hear firsthand what initiatives are contemplated, underway and recently completed.
Highmark Medical Services, one of Medicare’s Contractors, has amended its Local Coverage Determination so that NBDHMT certified CHT’s and CHRN’s are now able to conduct transcutaneous oxygen assessments, from a reimbursement compliance standpoint. For many years, it was only certified vascular technologists or those working in a certified vascular laboratory that met Medicare reimbursements compliance criteria. We were able to convince several contractors that it made good sense to extend authorization to hyperbaric team members. Over the ensuing 15 years several key Contractors have agreed. On January 12, 2012, Highmark became the latest. It was this evolution within the Medicare system that had prompted the NBDHMT to formalize training and certification standards related to transcutaneous tissue oxygen tension measurements. To determine if your region’s Medicare Contractor permits hospitals under its jurisdiction to file claims for transcutaneous oxygen testing by those in the hyperbaric medicine facility check with your prevailing Local Coverage Determination for Non-invasive Peripheral Vascular Studies Lower Extremity Arterial Testing.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2012
The Board was saddened to learn of a recent (February 10) hyperbaric chamber accident with resultant loss of life. The preliminary police report notes that a lone horse was being treated. It was still shod and was not wearing protective shoe covers. Some 20 minutes into the treatment the horse began to act up. It kicked away the protective cover exposing the chamber’s steel hull. The horse continued to kick the hull with its metal shoes, eventually causing a large spark. A fire was observed soon thereafter. As the chamber operator began to decompress the chamber a survivor described hearing a small explosion followed by a much larger one that caused catastrophic structural failure. The larger explosion was apparently heard 30 miles away. The horse did not survive nor did the chamber operator and survivor was air-lifted to the University of Florida Shands Hospital trauma center. The Board’s condolences are extended to the family of Erica Marshall and we wish Sorcha Moneley a speedy recovery.
While oxygen is not combustible, per se, it readily supports combustion. So, when the spark was generated, then would need for a fuel to ignite and burn. We do not know the composition of the protective covering but, regardless, it is well known that flatulence from horses and other herbivores contains methane and hydrogen gases. These are two very flammable substances. The chamber was presumably compressed on oxygen; it is difficult to affect oxygen delivery via individualized systems for these animals in an air-filled chamber. If the chamber was not operating on a continual flush of oxygen basis then these gasses could accumulate. Why the resulting pressure increase would not have been controlled by the chamber’s over-pressure relief valve(s) cannot yet be reconciled.
The Board is hopeful that the events surrounding this dreadful event will be fully investigated such that any necessary future chamber design, operating policies and operator training will be optimized.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2012
January saw the successful completion of the first NBDHMT sponsored diver medic refresher training course. It was held in conjunction with the Association of Diving Contractors International ‘Underwater Intervention 2012’, in New Orleans. Speakers were a veritable ‘who’s who’ of the Gulf of Mexico diving medicine scene. Dr.’s Van Meter, Sirio, Bourgeois, Alleman, Murphy-Lavoie, LeGros and Buford joined Cal-Dive Int.’s Health and Safety Director (and NBDHMT Executive Committee Member) Terry Overland, Safety Management Systems Chris Peppler, and this writer. Two full days were packed with reviews and updates on decompression illness, barotraumas, marine life injuries, case management scenarios and ‘lessons learned’ from past accidents. A series of interactive case presentations and several hands-on clinical skills stations rounded out the course.
All of the speakers willingly gave of their time and expertise and did so without expectation. They freely interacted with attendees during didactic and practical sessions. The quality of the speakers and their material was not lost on the attendees. Early and enthusiastic feedback was sufficient to warrant this course becoming an annual event.
On Friday, January 27, the first Beta testing of the new DMT certification was undertaken. A total of 22 recently graduated diver medics from courses in Key Largo, Florida (The Aquarius Seabed Laboratory) and Denver, Colorado, agreed to take part in this process. Several other DMT training programs will join assist in this manner over the next several months. Results are being fed back to DMT teaching teams so that they can fine tune respective course content in order to address any perceived weaknesses. The Board’s goal is to introduce this standardized examination by the end of 2012.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2012
The year 2011 was both eventful and encouraging. It was eventful in that the Board successfully introduced a new certification program in hyperbaric veterinary technology. It was encouraging in that despite these difficult economic times the Board’s finances are in better shape than at any other time. This improvement has placed Board in a position where it is able to provide financial support to independent mission-related safety and training initiatives. Earlier in the year a grant was provided to a group that is developing a hyperbaric materials safety testing program. Funds have also been made available to sponsor a DMT refresher training program (scheduled for January 25/26, in New Orleans).
Other notable events include, sadly, the passing of long-standing Board member Bill Hamilton and the recruitment of three new Board members.
This year kicks off with Beta testing of the DMT certification examination. As previously mentioned, the goal of this process is to bring DMT certification in line with that of the CHT, CHT-V, and CHRN programs; namely, that a standardized exam be used. At present, a DMT student becomes automatically eligible for DMT certification upon successful completion of a DMT training course. There is currently no direct oversight by the Board and places some strain on this program’s credibility. Soon, a standardized examination will be independently administered and proctored, as is the case with the three other certification programs. Later this month, Beta testing will take place following DMT training courses in Florida and Colorado. Additional testing will occur at several other sites throughout the first half of the year. From that point on it is anticipated that all subsequent applicants for DMT certification will be required to take the standardized exam. Below is a link to a summary of the various sections that comprise the exam and the degree to which each section constitutes to its overall 120 questions. As with our other certification examinations there are several exams variants, each drawn from the question database.
Happy New Year!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2011
December 2011
I am pleased to welcome three new members to our Board of Directors. They are Michael Powers, CHT; Debra Gonzalez, RN, ACHRN, CHT and Valerie Short, RN, ACHRN. Each brings a skill set, knowledge base and extensive experience in areas complementary to the mission and objectives of the Board. To learn more about our new members go to the ‘Who We Are’ link on our website. Brief biographical sketches have been posted.
A final reminder for all of you diver medics is that a DMT Refresher Training Course has been scheduled in January. It will coincide with the annual meeting of the Association of Diving Contractors International, in New Orleans. Course dates are January 25/26. Several undersea medicine experts have kindly agreed to donate their time. Safety Management Systems has been equally generous in their offer to provide an extensive invasive skills updating session during much of the second day. To learn more about this opportunity and to register please go to https://nbdhmt.org/dmt.asp.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2011
A reminder to all DMT’s that we have scheduled a refresher training opportunity early in the new year. It will take place in New Orleans on January 25/26 at the Ernest N. Morial Convention Center during Underwater Intervention 2012. I am pleased to report that this training opportunity will definitely take place as we already have sufficient registrants. An excellent line up of experienced diving medical specialists has been assembled. There will be didactic sessions and several invasive skill workshops with expert instructors and state-of-the-art manikins, both kindly provided by Safety Management Systems. Space is limited so register now at https://nbdhmt.org/dmt.asp if you plan to attend.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
October 2011
As you will have noted on our home page, we have lost a member of the board. R.W. ‘Bill’ Hamilton passed away in September after a brief illness. Bill served the interests of diver medics, hyperbaric technologists and hyperbaric nurses effectively, passionately and without expectation for over 15 years. But Bill’s ‘shadow’ extended far beyond his role with the NBDHMT.
Following service in the US Air Force as a fighter pilot during the Korean War and in Viet Nam (where he earned the Distinguished Flying Cross) he turned his attention from aerospace to the undersea. Throughout the next four decades Bill evolved into one of the world’s leading environmental and high pressure physiologists. His professional footprints are to be found through much of deep diving’s operational advancements and decompression processes. Upon joining Union Carbide Corporation he pioneered the initial laboratory ‘dives’ that led to the first manned saturation exposures on the continental shelf, exposures in excess of 600 fsw. He also pioneered the study of neon as a possible substitute for helium for dives in the 250-600 fsw range. It was during these research dives, in 1972, that I first met Bill. I was also one of the experimental subjects and we were compressed together to some 500 fsw. My task was to exercise on an ergometer while I was monitored and assessed for various biomedical and performance parameters. Being a fitness addict I sought to break the record for speed and distance on the ergometer bicycle. I did manage to but it came at great expense. During the subsequent decompression I suffered cerebral decompression sickness. It did not help that while passing 120 fsw the chamber operator inadvertently flushed the chamber with pure helium, not the intended helium-oxygen mixture. Bill likewise suffered decompression sickness in an extremity. I came out of it with permanent (right) hearing loss. Bill rushed home after a brief treatment as it was his anniversary and he had missed last year’s anniversary as he was likewise decompressing from a deep research dive.
Bill continued to pioneer decompression procedures, and contributed greatly to deep recreational technical and mixed gas diving. His decompression computer algorithms were acquired by numerous international navies and research laboratories.
Bill served in leadership and consulting capacities within the Undersea and Hyperbaric Medicine Society, the Divers Alert Network, the National Oceanographic and Atmospheric Agency, the National Fire Protection Association and the National Aeronautics and Space Administrations (NASA).
He was the recipient of awards too numerous to mention and leaves behind an enormous legacy. All of those who enter into, and work within, the ocean and other deep bodies of water are that much better off because of Bill. To say he will be missed somehow seems quite inadequate.
Dick Clarke, President National Board of Diving & Hyperbaric Medical Technology
September 2011
This final report on the business conducted during the 2011 meeting of the Board of Directors relates to CHRN’s and CHT-V’s.
On the nursing front there are currently 377 CHRN’s, 80 ACHRN’s and 6 CHRN-C’s. In 2010 75 RN’s sat the nursing certification examination and 71 (95%) passed. Three of those who passed did so ‘With Distinction’, which meant they scored 90% or higher. During this same year 18 RN’s elected to sit the CHT rather than CHRN exam, with an overall success rate of 94%.
The veterinary hyperbaric technology certification program was discussed at length. All necessary program infrastructure is in place. At the present time, certification edibility will include attendance at a regular (CHT/CHRN) NBDHMT approved hyperbaric training course. It may well be that subsequent training courses will be created specific to vet techs, or veterinary technology components added to some of the existing hyperbaric training courses. Those members of the CHT-V certification committee who meet eligibility requirements will take the first test offered by the Board in the coming weeks.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
August 2011
In the July ‘Briefing’ I provided an update on Board of Directors Annual Meeting activity that was specific to the DMT program. This month I will do the same regarding the CHT program.
There are presently 1,377 active CHT’s. In 2010 the Board convened an impressive 51 testing sites for a total of 265 examinees. Of these, 75% passed (3% With Distinction). When reviewing the answers of those who did not pass there was a clear trend in incorrect responses. It appeared that little effort was made to review the relevant NFPA standards as they relate to overall hyperbaric operational and fire safety standards. Knowledge was also consistently lacking with regard to such fundamentals as air decompression procedures, pressure conversions and gas laws. Those who serve as preceptors for CHT interns are encouraged to direct interns to these areas so as to promote additional study emphasis. There is also a sense that those seeking CHT status are rushing to sit the certification examination before they have accrued sufficient operational experience to complement initial training and their 480 hours of preceptorship.
On another topic, the Board of Directors has posted a new Position Statement (July 2011; 2011-02). It relates to the not uncommon practice of having a pediatric patient accompanied in a monoplace chamber. The decision to require a staff or family member to join such patients is entirely that of the treating hyperbaric physician and presumably a decision based upon a risk-benefit assessment. It is not the intent of this latest Position Statement to argue the relative merits of this practice. Rather, the Board wants to ensure that should dual occupancy occur it does so with relevant safety standards considered.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
July 2011
The Board of Directors held its annual meeting in Fort Worth, Texas, on June 16. As has been common in the past, our Meeting coincided with the annual scientific meeting of the Undersea and Hyperbaric Medical Society. Here is an update on the Board’s discussions, as they related to the diver medic program.
There are presently 555 certified diver medics. Conversion to mandatory invasive skills training has been completed. ‘In-house’ certification testing will soon commence. Throughout the history of the DMT program diver medics who passed their post-DMT training course test were eligible for certification. The Board has long felt that insufficient oversight of the testing process was a flaw in the certification process. To bring the DMT program in line with the CHT and CHRN certification programs, the Board will soon assume responsibility for the testing of newly trained diver medics. Step one in this process will be to conduct a ‘sample’ testing at each of the Board approved training facilities. It will be a onetime process and results will not be applied to each student. Rather, their standard, post-course, test will be used for certification purposes. Once the Board’s sample test results have been compiled, each respective instructor/facility will be advised of any topics that require addition emphasis during future training courses. From this point forward, the Board’s examination will be in force for all subsequent DMT certification eligibility. The Board’s examination guidelines can be viewed at the ‘Diver Medics’ link on the website, and listed as item #7. Here you will see that the structure of the exam is broken down into seven categories. A description of each category’s content is included, as well as the relative percentage of topics and questions that each category contributes to the overall examination.
DMT training standards were also discussed, particularly in light of the new certification examination. The Board remains keen to ensure that everything possible is done to produce a high value DMT resource. To that end we will be again be meeting with physicians, supervisors and safety officers in New Orleans at the time of the Association of Diving Contractors International conference next January. In subsequent ‘Briefings’ I will update each of the other certification programs.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
June 2011
You may recall the report earlier this year of a devastating horse barn fire at a Texas training facility. The fire claimed the lives of 25 of the 32 horses stabled there. One highly regarded horse, ‘Keep On Smoking’, suffered second and third degree burns. He was transferred to an equine sports medicine and surgery facility, in Weatherford, Texas. This facility includes 24/7 critical care and hyperbaric oxygen therapy. ‘Keep On Smoking’ underwent 12 hyperbaric oxygen treatments as part of his burn wound management. He Tolerated them well and is expected to be fit to race again this coming September. And, no, the owners do not plan to change his name!
All of this has relevance to us now that the Board has added veterinary technology to its certification programs. Veterinary hyperbaric medicine is becoming increasingly common, involving both large and small animals. While most often rendered in a sub-acute setting, the above example indicates that urgent access to hyperbaric medicine is also necessary and as equally valuable as it is in humans.
CHVT testing begins this month, with the first examination scheduled to coincide with the UHMS Annual Scientific Meeting, in Fort Worth.
A reminder to those attending this meeting that we will again host a ‘Breakfast with the Board’ at 7:00 Friday, June 17. Drop by and meet the Board’s members.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
May 2011
You may have already noticed that a new link has been added to our website. It relates to certification in veterinary hyperbaric technology. Use of hyperbaric chambers to treat a number of different animal species has grown markedly over the past decade. In the US alone it is estimated that there are currently 30 such facilities. Those individuals who meet eligibility standards are now be able to become Certified Hyperbaric Veterinary Technologists (CHVT). As with the CHT and CHRN programs, it is anticipated that CHVT’s will serve to enhance safety and quality of delivered care. This new program should also go a long way in raising the stature and professionalism of veterinary hyperbaric medicine.
The annual meeting of the NBDHMT Board of Directors is just around the corner. It is scheduled for June 16 and will coincide, as in the past, with the annual scientific meeting of the Undersea and Hyperbaric Medical Society, in Fort Worth Texas. For those planning to attend the UHMS meeting please join us for ‘Breakfast with the NBDHMT’. This popular annual event (and not just because it’s free!) is scheduled for Friday June 17 at 7:00 am. It represents an excellent opportunity to meet with members of the Board and hear firsthand what initiatives the Board is currently involved in and others that are planned. In order to expedite and streamline Board meetings they will no longer be open to non-Board members. However, the following morning’s breakfast will serve as an excellent opportunity for you to get updated, have your questions addressed and your comments heard.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2011
Evolution from Basic or Advanced DMT training and certification to only the equivalent of advanced status is complete. All those who certify and recertify as diver medics will process the necessary skill set required to comprehensively support the injured during recompression therapy. This has already done much to improve quality of delivered care. The treating physicians no longer have to worry about on-site inability to manage the airway, provide fluids and medications through appropriate invasive options, and cathertize the bladder.
The final component of two years of DMT training and certification enhancement is the centralization of the certification examination process. The electronic question bank is complete.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2011
The big news this month is that the certification program for veterinary hyperbaric technology is essentially complete. For the past two years a committee has worked diligently and without compensation to generate the training standards, certification eligibility requirements and examination question bank, for those who provide hyperbaric oxygen therapy to a wide animal species. This form of hyperbaric oxygen therapy has grown enormously over the past decade, in the US and elsewhere. It has not been incident free. There have been several fires with resultant loss of life.
It makes sense, therefore, that those who operate animal hyperbaric should be trained and certified to the same level that is expected of human operations. The Board expects to begin certification testing for CHT-Vet status in the summer. Leading the veterinary hyperbaric certification process was Dr. Dennis Geiser, who also chaired the certification development committee. In recognition of his unselfish and energetic commitment to this new program and to ensure representative balance, Dr. Geiser has been elected to the NBDHMT Board.
Dr. Geiser serves as Assistant Dean for Organizational Development and Outreach, and Interim Department Head – Large Animal Clinical Sciences, at the University of Tennessee, Knoxville. Dr. Geiser is highly regarded within the field of veterinary medicine. He has co-edited two textbooks, authored six textbook chapters, and has many other publications to his credit. The Board is honored and delighted to have longer term access to Dr. Geiser’s wisdom and insight.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2011
As is our standard practice, we have scheduled our 2011 meeting of the Board’s directors to coincide with the Undersea and Hyperbaric Medical Society’s annual meeting. This year it will be held in Ft. Worth Texas, June 15-18. If you plan to attend please be sure to join us on Friday June 16, for another ‘Breakfast with the Board’. This get- together offers an excellent opportunity to meet our directors and learn firsthand of initiatives we have planned or currently underway.
A big thank-you is in order to Laura Josefsen. Laura has served on the NBDHMT as a member of the Board’s Executive Committee for many years and has been a helpful resource. She recently became the nurse-elect to the Board of Directors of the Undersea and Hyperbaric Medical Society. To best devote her time to the needs of this new position she has resigned from the Board’s directors. We wish her well. Replacing Laura on the Board’s Executive Committee is Terry Overland. Terry has likewise been a long-standing member of the Board. He is our eyes and ears on all things commercial diving and the diver medic.
Dick Clarke, CHT, President
National Board of Diving & Hyperbaric Medicine
(top
January 2011
I want to take this opportunity to advise you of a new and important hyperbaric chamber fire safety initiative. This initiative has been born from the increasing number of patients undergoing clinical hyperbaric oxygen therapy. These patients present with an ever expanding number of supportive biomedical devices, both implanted and otherwise. They present with an array of wound dressings and wound products. Many of these dressing contain active ingredients aimed at stimulating wound repair.
Little is known about the majority of these products and agents as they relate to hyperbaric chamber compatibility and risk of fire. To address this issue the Undersea and Hyperbaric Medical Society formed a ‘Material Testing Advisory Committee’. This Ad Hoc committee, chaired by NBDHMT Board member Richard Barry, has selected Wendell Hull & Associates (www.wendellhull.com) to develop standardized testing capabilities for evaluation of material compatibility for use within hyperbaric oxygen environments. The MTAC will work closely with Wendell Hull as they develop the testing process. The immediate goal of this initiative is to produce a set of established guidelines, recognized by an authoritative code writing body, for determining compatibility of an item before permitting its use within the hyperbaric medicine environment.
What is needed is a fund, estimated at $50,000.00, in order to complete this project and develop the necessary testing standards. The UHMS strongly endorses the project and will be responsible for its administration. However, because of its charter it is not authorized to solicit funding.
Institutions that provide hyperbaric oxygen therapy and organizations that work in support of the provision of undersea and hyperbaric medicine are encouraged to donate to this important hyperbaric safety cause. You will be pleased to learn that the NBDHMT, on behalf of its certified personnel, have made the first financial contribution.
Donations should be marked ‘Hyperbaric Materials Testing” and sent to:
Wendall Hull and Associates
Attn: Gwenael Chiffoleau
5605 Dana Ana Road
Las Cruces, NM 88007
Dick Clark CHT, President
National Board of Diving & Hyperbaric Medical Technology
2010
December 2010
We are just wrapping up our first year of mandated preceptorship of CHT internships. It is appropriate, therefore, for the Board to express its appreciation to all of the CHT’s and CHRN’s who have volunteered their time in this regard. Those 40 hours of direct oversight go a long way to enhancing the experience and capabilities of each new certified hyperbaric technologist.For those of you, who have not offered your services but would like to do so, please notify Board headquarters. We are in great need of additional preceptors and you will be helping a great cause. Your compensation would not be financial, but something much more rewarding. You would be directly contributing to the quality of patient care within the unique discipline of hyperbaric oxygen therapy.
A reminder to, re-read the Boards Position Statements from time to time. They are, in the opinion of the NBDHMT, vital to the safe and effective provision of undersea and hyperbaric medicine. The Board welcomes any comments you may have relating to these positions.
Best wishes to you all for the coming holiday season. May your 2011 be safe, healthy and professionally rewarding.
Dick Clarke, CHT, President
National Board of Diving & Hyperbaric Medical Technology
November 2010
On October 11, 2010 the American College of Hyperbaric Medicine circulated a press release regarding the National Board of Diving & Hyperbaric Medical Technology. It implied that the NBDHMT had only recently joined the ranks of those who have adopted on-line continuing education. The release went on to market one of their meetings, suggesting that CHT’s and CHRN’s could receive their recertification CEU’s by on-line or physical presence. The Board advised the ACHM that contrary to their assertions, the NBDHMT had actually pioneered on-line hyperbaric and undersea medicine education a decade ago, and as they had not applied for CEU’s for the meeting in question their indication the CHT’S and CHRN’s could gain necessary credits was likewise incorrect. We asked the ACHM to post a corrective follow-up release generated by the NBDHMT. The ACHM failed to do so as the Board requested, so we have done so ourselves, a copy of which in reproduced below.
NBDHMT Requested Release:
In follow-up to our recent memo regarding the NBDHMT, on-line education and the Board’s provision of educational credits, we heard from Mr. Clarke, Board president. He pointed out that contrary to our assertion that the Board had recently recognized and adopted on-line education; the NBDHMT had actually pioneered this process as it relates to the discipline of undersea medicine and hyperbaric oxygen therapy. This continuing education opportunity, Mr. Clarke noted, has been in place for much of the past decade. Mr. Clarke added that he was instrumental in getting the Undersea and Hyperbaric Medical Society to adopt enduring materials with on-line continuing educational credits in the early part of the past decade. Mr. Clarke also wanted the ACHM to emphasize in its various communication tools that the NBDHMT does not approve on-line introductory hyperbaric training courses as a method of entry level training and as a pathway for certification as a CHT or a CHRN. Consistent with the UHMS, the Board requires entry level training in hyperbaric medicine to be conducted in a face to face setting at its approved training facilities.
October 2010
The Board continues to heighten the quality of its certification products. Position statements posted on our web site make very clear the Board’s intent as it relates to specific safety and practice quality expectations and areas of potential controversy. As these statements frequently involve the larger discipline of undersea and hyperbaric medicine we are pleased to see that they have been reproduced or referenced by other professional organizations. The Board invites you to forward any questions or comments you might have about our various positions. Your feedback may well result in the publication of additional such statements.
The recently introduced, Code of Conduct has been broadly and positively embraced. We have received just one complaint from all 1221 certified hyperbaric technologists. Employers are expected to gain a measure of assurance that licensing and certification practice standards common across the health care delivery system are now inclusive of the hyperbaric technologist. Every applicant for CHT status is required to sign the Code of Conduct as a component of their examination eligibility criteria. All existing CHT’s will likewise be required to do so as they apply for recertification.
Effective August 1, 2010, nurses applying to sit the CHRN certification examination are now required to undergo a criminal background check. Background checks were initially limited to CHT’s as state licensing boards traditionally included nursing background checks. This is no longer the case in some states so the Baromedical Nurses Association Certification Board has directed the NBDHMT to institute this process as of the above date.
The chief beneficiary of these program enhancements, of course, is the patient, who deserves nothing less. Their collective impact, however, can be expected to extend to our professional colleagues, as well as the broader health care industry. And that is a good thing too!
Dick Clarke, CHT, President
National Board of Diving & Hyperbaric Medical Technology
September 2010
To all of you who have already returned your signed CHT Code of Conduct, many thanks! The Board is very encouraged by the sheer number of responses given that the Code of Conduct declaration is not actually required until your recertification application. We take this as an indication of your respective commitment to ethical conduct, integrity and honesty
For those CHT and CHRN’s unable to attend meetings and conferences that award educational credits it can be difficult to meet the necessary continuing education requirements for recertification. It might be helpful to learn, therefore, of several on-line programs that are approved by the NBDHMT for both Category A (directly related to undersea and hyperbaric medicine) and Category B (indirectly related; topics such as ACLS and BLS, infection control, HIPAA issues, hospital competencies are examples) credits. They can be accessed at:
http://www.woundeducationpartners.com/
http://www.mededonline.org/
http://www.wendellhull.com
On a final note I would like to express my appreciation to Jeannie McLamb. Jeannie was instrumental in the seamless relocation of NBDHMT headquarters from New Orleans to Columbia in May of last year. Many of you will have communicated with Jeannie in her capacity as Board Administrator over the ensuing 17 months. Jeannie and her family will be relocating to Dallas, Texas in the early part of this month. I would like to thank her for her efforts to enhance the quality of the Board’s functions and on your behalf I wish her well.
Dick Clarke, CHT, President
National Board of Diving & Hyperbaric Medical Technology
August 2010
Effective August 1 of this year a CHT Code of Conduct has been introduced. This development reflects a growing broader acknowledgement that professional activities cannot be regulated by legislation alone. Codes of Conduct are now to be found within federal and state governments, the finance industry (and not before time!), commerce, academia, and various nonprofit organizations. By committing to a specific code of conduct, individuals agree to the incorporation of moral and ethical standards into their professional behavior.
From this point forward, all new applicants for CHT status and those applying for renewal will be required to sign the NBDHMT CHT Code of Conduct. The Code is reproduced below.
As a NBDHMT Certified Hyperbaric Technologist I, the undersigned, acknowledge and agree to honor my obligations to observe the highest standards of ethical conduct, integrity and honestly. Further, I agree that in the performance of my duties:
- I will conduct myself in a manner that reflects positively on the NBDHMT and the hyperbaric medicine discipline in general
- I will refrain from behavior that harms the public and professional perception of the NBDHMT and the hyperbaric medicine discipline in general
- I will conduct my employment consistent with all applicable rules, regulations and laws to which health care providers in general and hyperbaric medicine personnel in particular are subject
- I have read all of the NBDHMT published ‘Position Statements‘, understand their intent, and commit to remaining current as new ‘Position Statements‘ are promulgated
- I will promote adherence to all relevant facility and patient safety aspects described within the NBDHMT’s ‘Position Statements‘
The Board is confident that the introduction of this moral and ethical commitment will enhance the standing of the CHT program and its certifying organization. It should also serve to improve the quality of care delivered to our respective patient populations.
Dick Clarke, CHT, President
National Board of Diving & Hyperbaric Medical Technology
July 2010
The NBDHMT Board of Directors held its annual meeting in St. Petersburg, Florida on June 2, 2010. As in common, it coincided with the Undersea and Hyperbaric Medical Society’s annual scientific meeting.
Several immediate items arising from the meeting that would be of interest are listed below.
- Despite the unusually high costs associated with the relocation of the Board’s headquarters from New Orleans to Columbia, SC, the associated upgrading of office technologies and conversion to a largely paperless process our financial health remains very good.
- The term “qualifying vocation” has been changed to “qualifying pathway”. This is largely semantics but does more accurately reflect the process by which each CHT applicants professional eligibility is considered.
- A DMT is not a qualifying vocation/pathway for CHT. To qualify as a CHT one must have completed an NBDHMT approved hyperbaric medicine training course. Certification as a DMT is based upon completion of a diver-medic training course. These two training processes address very different goals and objectives.
- A Board administered DMT certification examination remains on track for early 2011. Board approved DMT instructors will be kept updated as this initiative nears completion.
- A record 45 CHT and CHRN testing sites were convened over the past 12 months.
- A CHT certification program in veterinary technology continues to evolve. This initiative is headed up by Dennis Geiser, a veterinary surgeon based in Knoxville, TN. He attended the meeting and updated his committee’s progress. We are aiming for the first examination in 2011.
A number of other decisions were made and a series of “Action Items” established. I will continue to update you on these and other events by way of these Monthly Briefings.

On a final and particularly sad note, I want to advise you that Pauline Poletti passed away recently. Pauline had suffered cancer for a little more than a year and had done so bravely. As many of you will appreciate, Pauline was a huge part of the Board’s administrative activities for almost two decades. She was fiercely loyal and had absolute “ownership” of her responsibilities and duties. She was uniformly considered helpful and supportive by all those who interacted with her on certification and related matters. The Department of Defense did fly her son home from the Middle East to be by her side in her final days. The Board of Directors extends its deepest and heartfelt sympathies to Pauline’s family during this difficult period.
Dick Clarke, CHT, President
National Board of Diving & Hyperbaric Medical Technology
June 2010
The Board is increasingly concerned with what appears to be the practice of hyperbaric oxygen therapy without appropriate physician oversight. It is particularly disturbing to learn that, in some cases, it is the CHT’s who is operating a hyperbaric treatment facility in the absence of a physician. Disturbing, given that the process of preparing for and taking the hyperbaric certification exam offers ample evidence of wide – ranging complications and side effects that may complicate patient care. Such problems clearly require physician directed diagnosis, interpretation and management.
Please take a moment to read, or re-read, the Board’s Position Statement number 2010-01, posted in April of this year. You can locate it on the Board’s Home Page. This statement makes The Board’s expectations regarding the operational practice of hyperbaric medicine very clear. Our patients deserve nothing less.
Dick Clarke, CHT, President
National Board of Diving & Hyperbaric Medical Technology
May 2010
As the pace of the Board’s activities continues to accelerate we want to improve the way we communicate important developments. The “Monthly Briefing” does receive some 440 visits every month. This is encouraging. However, a larger number of our diver medics, technologists and nurses do not access and benefit from this content, given that we have 4,000 of them!
To better spread the word then, we plan a monthly email blast. It will contain the current month’s briefing, along with anything else deemed informative. Examples of which will include the latest Position Statement, any significant changes to the certification and recertification processes and introduction of any new programs – the veterinary hyperbaric technologist certification is working its way to fruition.
You will have likely received our first blast, sent out during the last week of April. If not, we do not have your email address on file so send it in. The blast carried the Board’s most recent Position Statement (Physician Attendance and Supervision of Hyperbaric Oxygen Therapy). This statement was prompted by what appeared to be reports of CHT’s independently ordering and delivering hyperbaric oxygen therapy; ie, in the absence of a physician. To most of us this would be readily recognized as practicing medicine without appropriate licensure. It would further represent an obvious violation of several legal and regulatory standards and codes. However, the Board wishes to make this point very clear to its DMT, CHT and CHRN constituents.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
April 2010
I have some very good news to report regarding our diver medic colleagues serving in the U.S. Navy. In July of last year, at the invitation of Chief Petty Officer Blair Dell HMS, Special Operations Independent Duty Corpsman at the Naval Diving & Salvage Training Center and Diving Medicine for Medical Personnel lead instructor, I visited his program in Panama City. It was impressive, as was he. The diver medic training these guys undergo is both extensive and unparalleled. During my visit I was invited to speak to a DMT class about to graduate and another just getting underway. My topic was the history of the civilian DMT program and the role of today’s diver medic in the commercial diving industry.
This presentation started the wheels turning. Chief Dell and his colleagues began to research a pathway whereby naval personnel who complete DMT training could apply to the NBDHMT for civilian certification and be financially sponsored by the government. Step one was for us to review the USN DMT training course curriculum. As noted above, it was quite superb and greatly exceeded our minimum requirements. With course approval in place, these motivated individuals formally applied to the Department of the Navy for a civilian credentialing opportunity. This has recently been approved and I must say that the NBDHMT is honored to be able to certify graduates of their DMT program.
The annual meeting of the NBDHMT Board of Directors is on the horizon. As in the past, it will coincide with the annual scientific meeting of the Undersea and Hyperbaric Medical Society, in St. Pete, Florida (June 3-5). A reminder that if you are planning to be there, then don’t miss ‘Breakfast with the Board’. This year’s breakfast will be at 7:00am on Friday, June 4, 2010. Try to make it. You will have the opportunity to meet personally with the Board and learn what we have planned for the coming year. At this year’s meeting we will also have an exhibitor booth so please drop by and say hello.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
March 2010
Our efforts to provide advance notification of recertification deadlines by regular mail are frequently thwarted by incorrect postal addresses we have on file. It would be preferable, of course, to have everyone’s email contact. It is more likely to be up-to-date and avoids postal costs. We are in pretty good shape with all of you who have certified in the last several years. However, our records are less impressive for many who have been around a lot longer. Please ensure that the corporate office (nbdhmt@aol.com) has your email address when you have a moment.
Look our for us at the Undersea and Hyperbaric Medical Society Annual Scientific Meeting, June 3-5, in St. Petersburg, Florida, and Hyperbaric Medicine 2010, Columbia, South Carolina. We will have exhibitor booths at both of these meetings. Stop by and meet our administrative staff and Board Members. At the UHMS meeting we will again host a ‘Breakfast with the Board’. The Board’s certification activities will be updated as you enjoy a complimentary breakfast. This proved very popular last year, with some 70 in attendance. This is another good opportunity to get your questions addressed and represents a useful forum for comments and discussion.
Recent visitors to the Board’s website will have recognized a new logo. Nurses now have clear representation on the Home Page via very nicely designed imagery. With the development of a CHRN specific logo we have been able to introduce merchandise specific to the certified hyperbaric nurse. Check out these and several other additions to the Online Store link using the link provided on the Home Page.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2010
With the elimination of the Basic level DMT. There exists a need to access invasive skills training. A survey of DMT instructors indicates that such opportunities do exist. The following facilities/instructors have indicated interest in a ‘bridging’ course that will provide the necessary training to permit Basic DMT’s to re-certify.
Hyperbaric Training Associates/Ron Ellerman
rellerman@wi.rr.com
Oxyheal Health Group/Kevan Corson
kcorson@oxyheal.com
Divers Alert Network/USC Catalina Hyperbaric Chambers
huggins@usc.edu
National Polytechnic College of Science
jspelich@natpoly.edu
Contact those instructors if you need additional information. Effective January 1 of this year invasive skills are a mandatory component of the DMT certification training curriculum.
The Board recently decided to eliminate two of the long established CHT Qualifying Vocations. One was ‘Researcher’. This was rather a vague term. It had very rarely been employed during certification requests and it did represent a potential for abuse of the spirit and intent of the Qualifying Vocation. The second was ‘Medical Services Specialist’. This is a title and position specific to military personnel. Again it has very rarely been employed. Should medical services specialist wish to apply for CHT status, alternative Qualifying Vocation pathways exist (EMT or application to the ‘Others’ subsequently appeal to the Board).
A reminder that the 480 hours of preceptorship that follows hyperbaric training must include 40 hours of direct oversight. Established CHT’s and CHRN’s are expected to serve in this capacity. Specific preceptor guidelines will appear in the March Briefing. Hyperbaric physicians would represent an alternative, should there be a program lacking experienced technologist and nurses. If difficulties persist please contact Board headquarters.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2010
Adding to NBDHMT recognition by the Health on the Net Foundation as promoting useful and reliable information, the NBDHMT is now a proud member of the Institute of Credentialing Excellence. Formerly the National Organization for Competency Assurance, ICE is dedicated to providing education, networking and advocacy resources for the credentialing community. We will be submitting applications for our DMT®, CHT® and CHRN® credentialing programs to ICE’s accrediting body, the National Commission for Certifying Agencies, in the coming months.
We are going to delay the restructuring of the DMT® certification examination. You may recall that the Board had intended to align DMT® certification testing with its CHT® and CHRN® processes. This was to have occurred on January 1 of this year. Unanticipated delays in the reconfiguring of the exam question bank have necessitated this change in plan. All of the Board’s approve DMT® instructors and DMT® training facilities have been advised to maintain their current testing procedures until further advised.
Progress continues with the development of a certification examination in veterinary hyperbaric technology. Under the able leadership of Dr. Dennis Geiser, DVM, University of Tennessee, College of Veterinary Medicine, a committee is fine-tuning the process where those seeking such certification will be trained, tested and credentialed. It is anticipated that Board approved training will commence before the end of this year.
As the Board enters it 25th year I am reminded of its formative period. Having first attempted, unsuccessfully, to align certification of diver medics with the National Registry of Emergency Medical Technicians, the Board was formed in 1985. We were advised by some at that time that an upstart organization such as ours would fail to gain necessary credibility and respect. Time has proven otherwise. And all of those who have benefited therapeutically from your care, be they the commercial oilfield saturation diver off Brasil’s Atlantic coast, the teenage female scuba diver in the Florida Keys, the carbon monoxide poisoned warehouse worker in Salt Lake City or the retiree in Philadelphia who avoided losing her radiation damaged bladder, represent the ultimate validation of a certification body dedicated to the safe and effective application of undersea medicine and hyperbaric oxygen therapy.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
2009
December 2009
Take a moment to check out the Board’s all new Online Store. It was completely revamped and upgraded in November. Merchandise is of the highest quality and the store’s payment process has finally entered the modern era — credit cards are accepted! Consider these items as a great way of displaying and promoting your certification status as a Diver Medic or Hyperbaric Technologist. Hyperbaric Nurse merchandise will be offered once a suitable logo has been designed and approved by the Baromedical Nurses Association Certification Board. Let us know if there are other items you would like to see offered. Sweat shirts and ball caps are in the works.
A new NBDHMT Position Statement was posted on the website home page several weeks ago. It relates to the disturbing practice of hyperbaric oxygen chambers and related supportive infrastructure being sold to the lay public and used in the in-home setting. To the informed, this practice will immediately raise several red flags. Given the Board’s leadership position on all things hyperbaric safety, it would be remiss if we did not offer public comment against this practice.
This month’s ‘Briefing’ represents a full calendar year of what we hope have been helpful insights. We will continue to use this communication vehicle to keep you apprised of what we have in the planning stages and what is being contemplated. Those of you who have written to us about the Monthly Briefings have been uniformly pleased. We hope this sentiment extends more broadly.
Some reminders: The decompression table’s examination questions on both the CHT and CHRN examinations will change effective January 1. From this point, these questions will be based upon the most recent version of the U.S. Navy Diving Manual (Revision 6). All DMT training must incorporate invasive skills training in the new year. Fees will increase for CHRN certification on January 1st, 2010.
DMT certificates will be issued only at the time of the initial certification. A new card will be issued upon re-certification. In the past, certificates were issued for both certification and re-certification. We have updated the certificates so they no longer have an expiration date. Therefore, your certificate will always show your original certification date.
On a final note, Board Administrators Jeannie McLamb and Nancy Martinich join me and the entire Board of Directors in wishing you and your families an enjoyable and safe holiday season.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
November 2009
Many of you will have noticed the HON icon that now features prominently on the Board’s website. The Health on the Net Foundation (HON) promotes and guides the deployment of useful and reliable health information. Created in 1995, HON is a non-profit, non-governmental organization. It is accredited to the Economic and Social Council of the United Nations.
The NBDHMT received HON certification in October of this year. This important distinction was the result of a HON review committee determination that the information contained within the NBDHMT website meets HON’s eight ethical principals. HON will regularly monitor the website to ensure ongoing compliance. Visitors to the site are assured of the quality and trustworthiness of its medical and health content.
You may also have noticed improved navigation within the DMT, CHT and CHRN linked sections. The ability to locate and download certification application materials has been enhanced. Please don’t hesitate to contact Board headquarters if you feel that we can further enhance the value of our website content.
As noted in previous ‘Monthly Briefings’, the Board has been researching the possibility of incorporating national testing centers into the certification examination process. Having completed the review process it is apparent that we will not be able to offer testing center examination options. Principally, it came down to cost. Clearly, these testing centers commonly deal with larger organizations than the NBDHMT. Unfortunately, there is no way that the Board can absorb associated annual costs (as high as $60,000 in two instances) nor realistically pass on these costs to those who sit the certification examinations. We will continue to coordinate on-site proctorship testing opportunities, to the widest geographic scope possible. A quick review of the current testing locations will indicate just how wide spread and how frequent the Board is able to schedule testing sites. For 2009 alone, some 30 locations will have been used by the end of the year.
On a final note, a new CHT certification level has been introduced. It serves to recognize those who have advanced professionally from their technical and clinical duties to management and administrative responsibilities. Until now, these individuals have frequently been unable to complete the necessary technical and clinical hours to meet CHT recertification requirements. By applying for CHT-Admin, they will now be able to maintain their CHT ‘identity’ and continue to be recognized as a hyperbaric professional.
October 2009
‘Primary Source Verification’ is now live on our website for all categories of certification. Prospective employers can now directly search our CHRN, CHT and DMT databases. Upon entering an individual’s last name in the appropriate box, via the ‘Confirm Certification’ link on the Home Page, one will see that individual’s full name, certification number (for CHRN’s and CHT’s) and expiration date, if they are indeed certified. Each of the three databases is updated weekly. If the name of a particular individual does not appear, those searching are prompted to a link to the Board headquarters email address to request a more updated search.
Animal chambers have long been a part of hyperbaric medicine’s research efforts. More recently, animal chambers have been employed in a clinical/treatment setting. This practice is growing considerable, and on an international scale. Some of the conditions suffered by our hyperbaric patients are also suffered by animals. One would expect, therefore, that these animals would derive benefits similar to those our patients enjoy. Already, however, there have been several fatal equine hyperbaric chamber fires. In order to enhance the practice safety and clinical effectiveness of these animal chambers, the NBDHMT is in the process of developing a hyperbaric certification standard for veterinary technologists. A working group made up of NBDHMT Board members and veterinary specialists has been formed. Their remit is to create a training course and certification examination that will result in the awarding of a Certification in Hyperbaric Veterinary Technology (CHVT). It is intended that this new NBDHMT certification will be available in the latter part of 2010.
On a final note, certification and recertification fees for CHRN’s will increase on January 1, 2010. The Board will accept payment at the current rates for 2010 certifications if payments are received by December 31 of this year. For those of you due to recertify in the early part of 2010, payment in December will represent a saving of approximately 20% on next year’s fees.
September 2009
Certification examination schedules are at an all time high. From January through July of this year, testing was scheduled at 12 different locations, involving 105 nurses and technologists. For the remainder of the current year 16 additional examinations are scheduled, with 111 CHT/CHRN applicants registered to date. Independent of these impressive numbers is a steady volume of diver medics being certified.
Given the above, I thought that you might be interested to learn of the total number of those who have been certified since the inception of the NBDHMT. These numbers will provide some idea of the growing interest in the practice of undersea and hyperbaric medicine. The first CHT examination was offered in San Diego, in 1991. From that point, through 2005, 687 became certified. From 2006 to August 2009 another 702 have certified. The last four years, therefore, has seen more certification activity than in the previous fifteen years. On the nursing side, the CHRN exam was first offered in 1995. Through 2005, 292 nurses became certified. From 2006, an additional 326 have certified. Again, the last several years has produced more CHRN’s than the previous 11 years. The DMT certification program is equally impressive. While DMT training began in 1975, it was not until 1989 that formal certification was introduced. From 1989, through 2005, the Board certified 774 diver medics. In the last 3 ½ years another 839 have been added to the rolls.
I think that we can take comfort in this growth, and the increasing professional recognition and credibility that formal certification offers.
Work continues to restructure the DMT certification program into a single standard. As noted in previous briefings, the DMT testing process will be brought in-house in the coming year. The ‘Module 16’ training curriculum is being fine-tuned and the question bank finalized. The same applies to the adoption of national testing centers for three certification programs, which we hope to introduce in the not too distant future.
August 2009
The annual Board of Directors meeting was held in Las Vegas, in June, in conjunction with the 2009 annual scientific meeting of the Undersea and Hyperbaric Medical Society. An extensive agenda was tackled, much of it designed to enhance the operations and quality of the Board’s various certification processes.
Sub-committees were formed in order to upgrade the DMT training course outline (commonly referred to as Module 16) and to create the DMT examination database. As noted in early ‘Briefings’, the DMT certification examination process will be undertaken by the NBDHMT, in the same manner as the CHT and CHRN programs, beginning in 2010. Invasive skills training will become a standard component of all DMT training at that time.
Another important update is the decision to conduct all future certification examinations through a national chain of testing centers. This is now commonplace for medical, legal, accounting and other professions. The use of testing centers will make it much easier for individuals to schedule their exams, by not having to wait for the required minimum number of applicants before a test date can be scheduled in a specific area. It will also serve to enhance the security and confidentiality of the examination process. We expect to have this process in place by early 2010.
The Board has been approached by members of the veterinary medicine community. They are interested in the development of a training and certification standard for those who operate equine and other animal hyperbaric chambers. An initial approach occurred two years ago; interest is now renewed. I met with a representative of this group in July and the Board will look closely at this possible extension of its certification activities in the coming months.
The Board wishes to emphasize that, going forward, the 480 hours of preceptorship necessary to complete eligibility prior to taking the CHT examination must occur following formal Board approved hyperbaric training. Work experience that has been accumulated prior to the formal training is not considered part of the 480 hours of preceptorship. Preceptorships are expected to be undertaken via an experienced CHT or CHRN wherever possible. If you are thinking of becoming certified in hyperbaric technology, please have your preceptor contact the Board for a guidance document.
On another topic, the Board wishes to clarify the procedure for those who fail their certification examination. They may re-take the examination following a six month waiting/study period. If an examinee fails a second time, they are then required to repeat formal NBDHMT approved hyperbaric training, at which point they become eligible to take the examination a third and final time. Those who fail their third attempt (and this has not occurred to date) would not be eligible to make any further attempts.
One final point is to remind those who apply for certification as CHT’s and CHRN’s that they must submit evidence of completion of three transcutaneous oxygen studies, which represents completion of the TCM Module training process. This evidence can be in the form of a statement within the letter that confirms completion of the preceptorship process.
July 2009
The new Board headquarters team continues to get a good grasp on the day-to-day aspects of the various certification processes. This has been enhanced by improved office automation capabilities and access to upgraded information technology. Your patience during the past several months has been greatly appreciated. We are now in a much better position to serve you more efficiently.
Both the upgraded CHT and CHRN examinations have literally been put to the test. It appears that our efforts to improve the respective testing banks have been successful. This observation is based upon the very few comments received with completed tests, which typically raise concerns regarding question clarity, appropriateness or intent. We will continue to monitor test results closely and make adjustments as they appear necessary.
If you are a certified DMT, CHT or CHRN and have not done so already, please take a moment to email the Board with your date of birth. We are in urgent need of this in order to introduce Primary Source Verification (see May 2009 Monthly Briefing).
A reminder that those DMT’s certified as ‘Basic” will need to provide evidence of invasive skills training upon application for re-certification on or after January 2010. In the coming months the Board will provide information on where such invasive skills training is being offered.
The NBDHMT Board of Directors held their annual meeting in Las Vegas, on June 24. This meeting coincided with the annual scientific meeting of the Undersea and Hyperbaric Medical Society. I will provide a summary of the Board meeting in the next edition of Monthly Briefing.
June 2009
Many of you will be aware of the fatal hyperbaric chamber fire that occurred in a free-standing facility in South Florida, on May 1st.
The fire appeared to involve an early model Vickers monoplace. While details of the resulting investigation have not yet been made public, early indications suggest that this facility’s normal course of operations involved marked violations from what would be considered standard hyperbaric safety. This tragic event has prompted the NBDHMT to move forward its planned publication of a series of Position Statements. The first two such Statements are now published on the Board’s Home Page. More will follow and any comments you may have are welcomed.
The Board’s headquarters are now operating from their new location, in Columbia, South Carolina. Please be patient as our team comes to grips with a huge amount of documentation. Note the new Board contact details at the foot of each page of the website. On a particularly sad note, I also want to let you know that the Board’s long serving office manager, Pauline Poletti, is seriously ill and unable to continue her employment. Pauline has a tough time ahead of her, yet she remains in good spirits. Not the least of her difficulties is mounting and uncovered health care costs. A fund has been established by her co-workers, family and friends to help offset these costs. If you would like to make a contribution to Pauline’s financial burden please send it to:
The Pauline Poletti Donation Account,
# 207 81 1600 8 at Capital One Bank.
Payments can be made directly to any Capital One Bank or sent to the attention of Mandy Wise, 1816 Industrial Blvd. Harvey, LA 70058-2314. I know that Pauline, who served the Board and all those who certified for almost 20 years, will be very grateful.
May 2009
Plans are underway to introduce ‘Primary Source Verification’ to the Board’s website. This is an increasingly common verification aspect of modern healthcare. It is now mandated by the Joint Commission on Accreditation of Healthcare Organizations for all clinical staff required by an employing organization, or the state, to have licensure, registration or certification. The purpose of this verification is to ensure that a person’s qualifications are consistent with their job responsibilities. In the past, such verification was a somewhat lengthy, convoluted and not always successful process. It commonly entailed hard copy communication with numerous related entities. Today the process can be greatly enhanced via access to information links within single website sources.
We plan to get the CHT verification process up and running first. Those seeking to confirm that a staff member or potential employee is currently certified in hyperbaric technology through the NBDHMT will be able to access the ‘Primary Source Verification’ link on the Board’s Home Page. By entering an individual’s name and date of birth, current certification status can be confirmed. We plan to have CHT verification in place by July of this year. Verification will be extended to DMTs and CHRNs in due course.
Another important news item is that the Board’s headquarters is being relocated to Columbia, South Carolina in the coming weeks. We anticipate a seamless transition and no interruption in certification and related support services. Look out for new contact details on the website. On behalf of the Board, I would like to extend my sincere thanks and deep appreciation to Dr. Keith Van Meter. He has generously provided an administrative home for the NBDHMT in his company’s offices in New Orleans for almost 20 years.
April 2009
An important milestone was reached during March of this year. The first major revision of the CHT examination in the 20 years since it was first introduced was completed. Questions have been added and deleted during this period. However, the exam was in need of a top to bottom overhaul and upgrading. What we have now better reflects today’s operational, technical and safety practice standards. The examination more effectively tests each prospective hyperbaric technologist’s core knowledge. Gone are the questions most relevant to nursing practice and hyperbaric physician decision-making. The examination has also been carefully weighted between key subject categories, in order to further improve balance specific to the roles and responsibilities of the hyperbaric technologist.
All subsequent CHT examinations will use this new question bank. We have elected to maintain the decompression tables’ questions based on the 1999 version of the U.S. Navy Manual’s Standard Air Decompression Tables for the time being. Many of you will be aware that these tables underwent a significant change in 2008. Theses new tables are now incorporated as Revision 6 of the U.S. Navy Diving Manual. We have elected to maintain the 1999 version as not all training centers have switched their teaching materials. We anticipate that the CHT examination will incorporate the 2008 decompression tables for all examinations that are scheduled after January 1, 2010. The principles of table computation remain the same. However, time frames have changed to reflect more conservative exposures and depths are now broken down into 5 instead of 10 fsw increments.
The Baromedical Nurses Association Certification Board is likewise undertaking a updating of the CHRN examination question bank. We expect that their new questions will be incorporated within the coming weeks and be reflected in all scheduled CHRN examinations after June 1, 2009.
March 2009
A recent visit to Board headquarters in February allowed me to reacquaint myself with Pauline and meet for the first time with Melissa. These two individuals are truly dedicated to the success of the Board’s mission and all those who certify. I also spent time with past president Paul Baker and executive committee member Dr. Keith Van Meter during my time at the office. We discussed a number of initiatives, one of which involves modernizing all of the present office technology. Another will see the Board being able to finally accept credit card payments.
I have a meeting scheduled with the diving medical officers and safety directors from the Gulf of Mexico’s commercial diving industry, in the early part of this month. The purpose of this meeting is to determine from these important ‘end users’ of the DMT certification program if we are continuing to meet their needs. Much has transpired in both the diving industry and the provision of emergency medical care since the inception of the DMT program, in 1975. The Board is presently undertaking a comprehensive review of the DMT certification program. We must ensure that it remains current, pertinent and responsive to the needs of the industry and its injured divers.
I am in communication with all of the current DMT training programs. They have provided valuable service over the years and we want to ensure that they have the necessary tools and guidance to continue to effectively address this important aspect of diving safety. Some changes are likely. The basis for any change will be enhanced education and training and the optimizing of care rendered on behalf of the injured diver.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
February 2009
From its independent beginnings, almost three decades ago, the NBDHMT has carved an indelible nitch within the mainstream of undersea and hyperbaric medicine’s safety and patient care consciousness. Early attempts to affiliate with existing certification bodies proved unsuccessful. The principal stumbling block was the operational, geographic and medical remoteness of the DMT. These diving first responders were, at times, far beyond the conventional time frames of traditional land-based EMT’s/Paramedics in terms of reaching medical facilities and transferring direct care to a physician. This perceived risk was considered too great a hurdle for pre-hospital certifying agencies to assume responsibility for the DMT.
Lacking any alternative and with a firm desire to standardize and enhance the DMT program, an independent non-profit organization was formed. Critic’s charged that such an organization would not gain the necessary credibility and acceptance. The board persisted. Time and events have proven our critics wrong. Today, the NBDHMT is an increasingly measured standard, in the U.S. and elsewhere. Oil and gas production companies, oil field diving support companies, hospitals, health insurance companies, training agencies, geographically remote recompression facilities and accreditation programs recognize and promote the personnel and standards that are a product of Board’s certification processes.
One recent and particularly important validation of the NBDHMT’s credibility and good standing in medical practice comes from Medicare, the U.S. government’s health insurance giant. Several of Medicare’s regional intermediaries are now mandating certification in hyperbaric technology or hyperbaric nursing in order to conduct reimbursable transcutaneous oxygen assessments outside of traditional vascular diagnostic setting. One such intermediary, Trailblazer’s Health Enterprises *, in a 2008 update, noted:
‘Additionally, transcutaneous oxygen measurements may be performed by persons possessing the following credential’s obtained by the National Board of Diving and Hyperbaric Medical Technology (NBDHMT):
Certified Hyperbaric Technologist (CHT) or,
Certified Hyperbaric Registered Nurse (CHRN)
* Trailblazer’s Health Enterprises, LLC
LCD Non-Invasive Peripheral Arterial Studies U-17B-R6; 10/01/2008
The board intends to build on all of this momentum. Stay tuned to the Monthly Briefing column to find out more specifically where we are heading.
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
January 2009
A note to say how pleased I am to return to the Board as its president and to advise you of some of the initiatives planned for the coming year.
It has been 13 years since I handed over the leadership reins to Paul Baker. Since then, and ably assisted by his fellow Board members, Paul has undertaken his duties and responsibilities to good effect. Now comes a well earned retirement – well, not entirely. I intend to appoint him to a Director-at-Large position. This will ensure continuity, as well as maintain the availability of a valuable resource.
Through a series of ‘Monthly Briefings’ posted on the website, I will keep you, the DMT, CHT and CHRN, in touch with the Board’s activities, initiatives and progress. In addition, you are invited to contact me at any time should there be other issues you would like to raise, or questions you may have. This first briefing will lay out what I have I mind as a starting point for my tenure.
I intend to initiate a detailed review of the DMT program. It has been in place for some 30 years and its graduates have played an important role, sometimes life-saving and often central nervous system sparing, in the practice diving medicine. This has particularly been the case in the medical and geographic remoteness of the commercial offshore diving industry. At this point in time I feel it important to ensure that the training and certification aspects envisioned and applied back in 1976 remain consistent with the evolving needs of the diving/undersea medicine communities.
To this end I plan to meet with safety officers and managers of the various commercial diving companies and diver treatment facilities in order to get their perspectives on the DMT program. It may also be preferable that we evolve to a ‘national’ DMT certification examination, as we have in place for the CHT program. Feedback from those who employ DMT’s will allow us to refine and upgrade related training standards and the certification process.
A second initiative will be to evaluate the potential ‘globalization’ of the Board’s certification activities through the teaming with similar organizations elsewhere in the world. Several opportunities already exist and others may be out there. Given our extensive certification experience, the Board is in a position to assume a leadership role as it relates to international diving and hyperbaric medicine safety, technology and practice excellence.
I will stay in touch with you through regular briefings that will be posted on the Board’s website. Best wishes for 2009!
Dick Clarke, President
National Board of Diving & Hyperbaric Medical Technology
Copyright © 2024. National Board of Diving and Hyperbaric Medical Technology. All rights reserved.
NBDHMT · P O Box 758 · Pelion, South Carolina 29123, USA · 888.312.2770
The National Board of Diving & Hyperbaric Medical Technology is a not-for-profit organization recognized as tax-exempt under the United States of America Internal Revenue Code section 501(c)(3) to ensure that the practice of diving medicine and hyperbaric oxygen therapy is supported by appropriately qualified technologists and nurses, through respective certification pathways. Funding is generated solely through certification fees and sales of Board merchandise. The National Board of Diving & Hyperbaric Medical Technology does not host or receive funding from advertisers or any other forms of business.
The information provided on this site is designed to support, not replace, the relationship that exists between visitors to this site and health care professionals. Any information collected by this site, such as e-mail address, will never be passed on to any third party, unless required by law.
Google Analytics is a webmaster tool used to determine the devices used to access this website so the content can be properly coded to serve phones, tablets or desktops. It is also used to determine the number of visitors to assess load on the server. It is used soley for this purpose and not configured in any way to track or individually identify the visitors themselves and should not concern the visitor in any way.
Updated April 1, 2024
